The Lump You're Ignoring: Why "It's Probably Nothing" Could Be Your Last Mistake
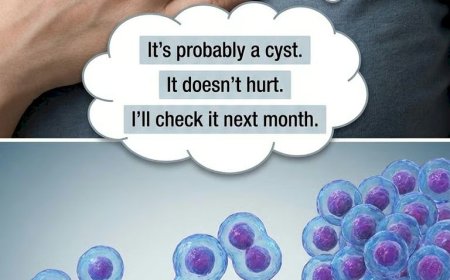
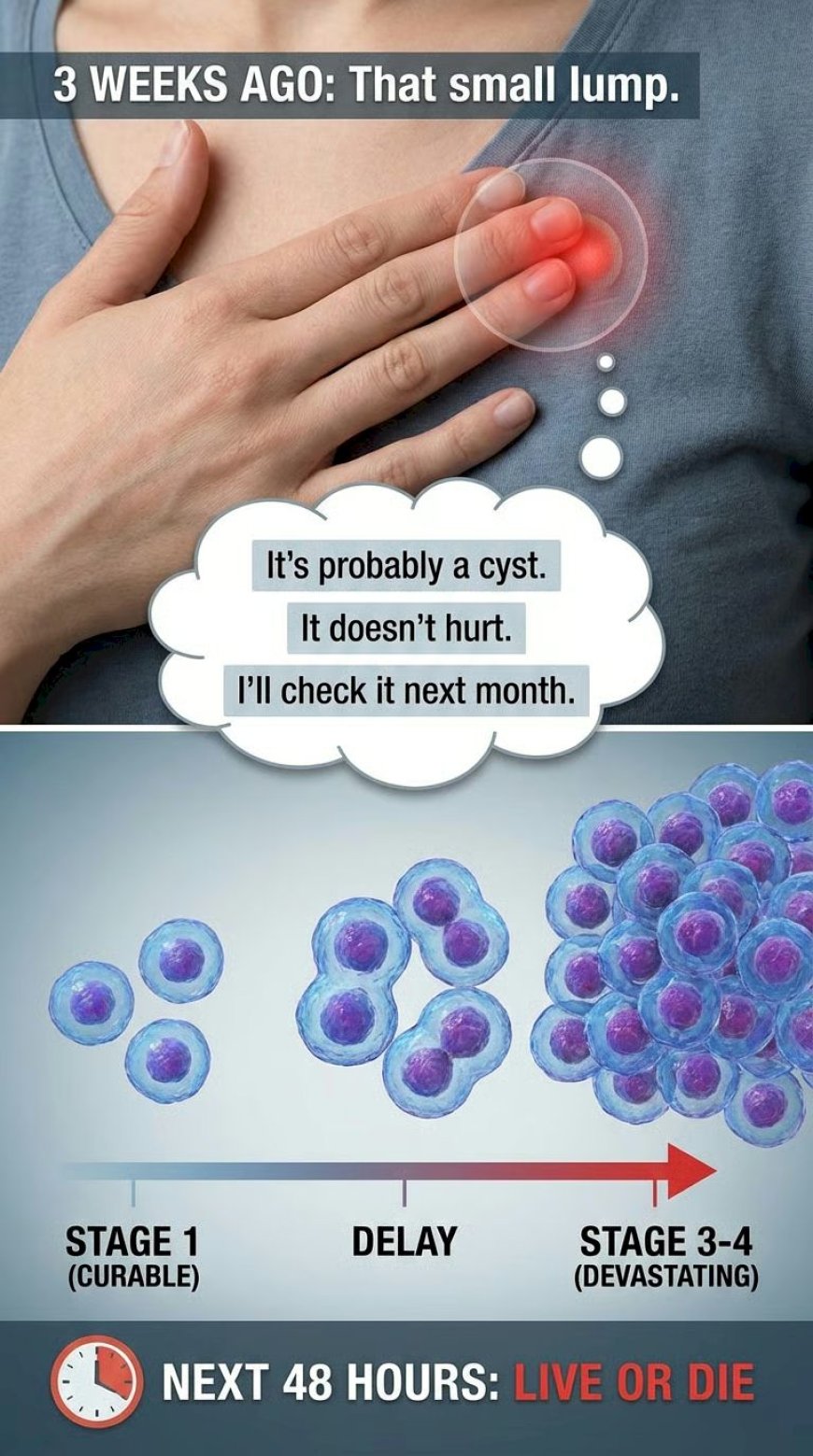
You felt it three weeks ago. That small lump. You told yourself it would go away. It's still there. Maybe bigger. And you're still making excuses. "It's probably a cyst." "It doesn't hurt, so it can't be serious." "I'll check it next month when I'm less busy." Every single day you delay, cancer cells—if that's what they are—are multiplying, spreading, moving from curable Stage 1 to devastating Stage 3 or 4. This article reveals why your brain tricks you into denial, what's really happening inside your body, and why the next 48 hours could determine whether you live or die.
The Moment Everything Changed (And You Almost Missed It)
Last Tuesday.
7:30 AM. You're in the shower.
Your hand brushes over your breast. Or your testicle. Or your neck.
There's something there that wasn't there before.
A lump. Small. Maybe the size of a pea. Maybe bigger.
Your heart skips a beat. Your breath catches.
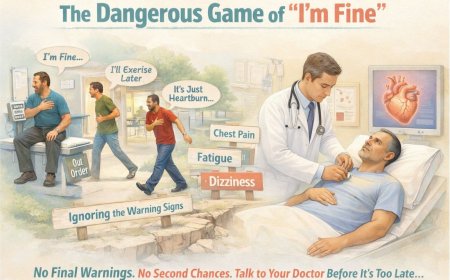
Then, within seconds, your brain kicks in with the rescue:
"It's probably nothing."
"Just a swollen gland."
"Maybe I slept on it wrong."
"I'll check it again tomorrow."
You finish your shower. Get dressed. Go to work. Convince yourself you imagined it.
But you didn't imagine it.
And three weeks later, it's still there. You've checked seventeen times. You know exactly where it is. You can find it instantly now.
Maybe it's even bigger.
But you're STILL not seeing a doctor.
Sound familiar?
Here's The Brutal Truth You're Avoiding
Right now, as you read this sentence, that lump is one of two things:
Option 1: It's benign. A cyst. A lipoma. A swollen lymph node from a recent infection. Something completely harmless that a doctor can confirm with simple tests, giving you peace of mind in days.
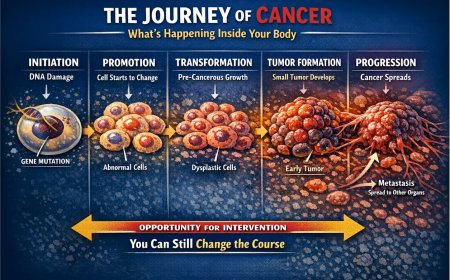
Option 2: It's cancer. And delays can allow cancer cells (if that’s what this is) to multiply and spread through the lymph system, potentially reaching distant organs.
Here's what you don't want to accept:
You won't know which one it is by touching it repeatedly in the shower, googling "does cancer hurt" at 2 AM, or convincing yourself that "if it was serious, my body would tell me."
The only way to know is to see a doctor. Get it examined. Get it tested.
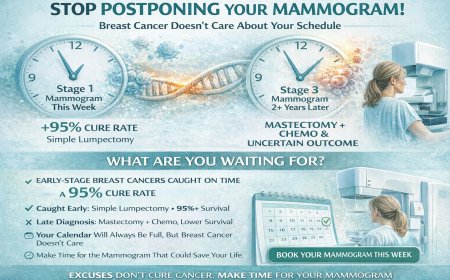
And the difference between finding out TODAY versus finding out months from now can be the difference between:
Stage 1 — surgery, possible cure, back to normal life.
Stage 3 — major surgery, chemotherapy, radiation, uncertain outcome.
Months. That’s all it can take for "probably nothing" to become "I'm so sorry, it's spread."
The Silent Rebellion Inside Your Body
Let me tell you what's happening inside your body right now if that lump is cancer:
Week 1–2: The False Peace
You found the lump. It's small. Doesn't hurt. You can move it around a bit. "See? Cancer lumps are supposed to be hard and fixed. This moves. It's fine."
Wrong.
Many cancers start as small, moveable lumps. Pain is not a requirement for malignancy. Your comfort is not an indicator of safety.
Inside: Cancer cells are doubling. One becomes two. Two becomes four. Four becomes eight. Exponential growth you cannot feel.
Week 3–6: The Dangerous Assumption
The lump is still there. You've noticed it hasn't gone away like you hoped. "But I feel fine otherwise. I'm not losing weight. No fever. If it was cancer, I'd feel sick."
Wrong again.
Early-stage cancer often has NO symptoms beyond the lump itself. That's why it's early. That's why it's catchable. That's why you MUST act now.
Inside: Cancer cells are establishing themselves. They're developing their own blood supply. They're preparing to spread to nearby lymph nodes.
Month 2–3: The Critical Window Closing
You've had this lump for three months now. You've finally admitted to yourself it's not going away. You're scared. So scared that you're doing nothing. Because finding out the truth feels worse than living in denial.
Inside: Cancer cells may have reached regional lymph nodes. What was Stage 1 could now be Stage 2 or 3. Treatment can become significantly more complex and uncertain.
Month 4–6: The Point of Potential No Return
You finally see a doctor. Months after first noticing the lump. The biopsy comes back.
"I'm so sorry. It's cancer. And it's spread beyond the primary site."
What could have been a simple procedure and surveillance may now be major surgery, months of chemotherapy, radiation therapy, and an uncertain prognosis.
And the worst part?
If you'd come in at Week 2, we might have caught it earlier. Early-stage outcomes for many cancers are often excellent; later-stage outcomes can be dramatically worse.
Those months of denial could cost you your life.
Why Your Brain Is Literally Protecting You to Death
Your Brain's Survival Mechanism (Working Against You)
Your mind is designed to avoid threats it can't immediately handle. Cancer is terrifying. Unknown. Potentially deadly. So your brain creates a defense mechanism: denial.
It convinces you that:
"It's probably just a cyst."
"Cancer lumps are supposed to hurt."
"I'm too young for cancer."
"It would be bigger if it was serious."
"I'll wait and see if it gets bigger."
Every single one of these thoughts is your brain protecting you from fear.
And every single one could kill you.
The "Doesn't Hurt = Not Serious" Fatal Mistake
This is the lie that kills more people than almost any other.
Most early-stage cancer lumps are PAINLESS.
Pain comes later — when the tumor is large, when it's pressing on nerves, when it's invading surrounding tissue, when it's advanced.
Pain is a LATE symptom, not an early warning.
If you're waiting for pain before you get checked, you're waiting until it may be too late.
Real Stories That Should Shake You Awake
Story #1: Priya, 34, Delhi
Felt a lump in her breast while getting dressed. Small. Didn't hurt. Moved slightly when pressed.
"I'm only 34. Breast cancer happens to older women. It's probably a cyst from my period. I'll check it after next month's cycle."
She waited four months. Finally told her mother, who brought her to a doctor.
Biopsy: Invasive ductal carcinoma. Stage 2B. The cancer had spread to 4 lymph nodes.
Treatment: Mastectomy. Six months of chemotherapy. Hair loss. Nausea. Fatigue. Permanent lymphedema in her arm.
Her words: "If I'd gone to the doctor at two weeks instead of four months, I might have kept my breast. I might have avoided chemo. I might not have this permanent swelling in my arm. Four months of denial changed everything."
The Five Deadly Lies You're Telling Yourself Right Now
Lie #1: "It doesn't hurt, so it can't be cancer"
The Brutal Reality: Most early-stage cancers are painless. Pain is often a LATE symptom when the tumor is large or invading nerves. Breast cancer? Usually painless. Testicular cancer? Usually painless. Lymphoma? Usually painless.
Painless lumps are exactly what you should be concerned about, because they are frequently the ones that prove to be malignant.
If you're using "no pain" as reassurance, you're using the wrong criteria.
Lie #2: "I'm too young for cancer"
The Brutal Reality: Cancer doesn't check your birth certificate. While certain cancers are more common in older populations, young people get cancer too. Testicular cancer primarily affects men aged 15–35. Breast cancer can occur in women in their 20s and 30s. Thyroid cancer frequently affects younger adults.
Age is not immunity. If anything, younger people sometimes experience more aggressive forms of cancer that grow faster.
Lie #3: "It moves when I touch it, so it's just a cyst"
The Brutal Reality: While fixed lumps are more concerning, moveable lumps can absolutely be cancerous, especially in early stages. As cancer progresses, it may become more fixed to surrounding tissue, but in the beginning, some cancerous lumps can feel mobile.
Mobility is not a reliable indicator of benign versus malignant. Only proper medical evaluation can determine this.
Lie #4: "I'll wait and see if it gets bigger"
The Brutal Reality: Waiting for a lump to grow before seeking medical attention is like waiting for a small fire to engulf your house before calling the fire department. If it's cancer and it's getting bigger, it's progressing. Cells are dividing. The cancer is advancing. Stage is increasing.
The best time to detect cancer is when it's small, not when it has grown large enough to frighten you into action.
Lie #5: "I feel fine otherwise, so it can't be serious"
The Brutal Reality: Early-stage cancer typically has NO systemic symptoms. You feel fine because your body has not yet been overwhelmed by advanced disease. Fatigue, weight loss, fever, night sweats — these come later, when cancer is more advanced.
Feeling healthy while having a lump is actually typical of early cancer. It is not reassuring; it is a window of opportunity you must not waste.
Understanding Different Types of Lumps
Not all lumps are the same. Here's what you need to know:
Breast Lumps
What to feel for: Hard, irregular lumps that don't move easily; skin changes such as dimpling, puckering, or redness; nipple discharge or inversion; and changes in breast size or shape.
Who's at risk: Women over 40 (but it can occur at any age), those with a family history of breast cancer, individuals with a personal history of breast conditions, and those with dense breast tissue.
Action required: Any new breast lump should be evaluated within 1–2 weeks, regardless of age.
Testicular Lumps
What to feel for: Hard, painless lumps on the testicle; swelling or heaviness in the scrotum; a dull ache in the lower abdomen or groin; and enlargement or tenderness of the breasts.
Who's at risk: Men aged 15–35 (peak incidence), those with a history of an undescended testicle, and those with a family history of testicular cancer.
Action required: Any testicular lump should be evaluated within days, not weeks. Testicular cancer is highly curable when caught early but can progress rapidly.
Neck and Lymph Node Lumps
What to feel for: Lumps in the neck, under the jaw, behind the ears, or in the armpits; hard, fixed lumps versus soft, mobile ones; lumps that persist beyond 2–3 weeks; and multiple lumps appearing simultaneously.
What might cause them: Infections (temporary swelling), lymphoma or other cancers, thyroid nodules or cancer, and metastasis from other cancers.
Action required: Lymph nodes that remain swollen for more than 2–4 weeks without an obvious infection should be evaluated promptly.
Skin Lumps
What to watch for: Rapidly growing lumps; lumps that bleed or ulcerate; changes in color, size, or shape; and lumps that feel hard or fixed to underlying tissue.
Possible causes: Lipomas (benign fatty lumps), cysts (fluid-filled sacs), melanoma or other skin cancers, and soft tissue sarcomas.
Action required: Any changing or concerning skin lump should be evaluated, especially if it appears different from other lumps you may have had before.
What Happens During a Medical Evaluation?
Many people avoid the doctor because they don't know what to expect. Here's exactly what will happen:
Initial Consultation (15–30 minutes)
The doctor will take your complete medical history, ask when you discovered the lump, perform a physical examination, document the characteristics of the lump, and discuss your concerns and symptoms.
Diagnostic Imaging
Depending on lump location, you may need one or more of the following.
For breast lumps: a mammogram (X-ray of breast tissue), an ultrasound (sound waves create images), or an MRI (detailed magnetic imaging) if needed.
For other lumps: ultrasound as the first-line investigation for most soft tissue lumps, a CT scan for detailed cross-sectional images, or an MRI for complex cases.
Biopsy (If Needed)
If imaging is suspicious or inconclusive, a biopsy will be recommended. Options include:
Fine Needle Aspiration (FNA): A thin needle extracts cells. It is quick, minimally invasive, and results are often available within several days (timelines vary by facility).
Core Needle Biopsy: A larger needle extracts a tissue sample. It is more definitive than FNA, with results often available within about a week (timelines vary by facility).
Excisional Biopsy: Surgical removal of the entire lump, which is both diagnostic and therapeutic, with results often available within 1–2 weeks (timelines vary by facility).
Results and Next Steps
If benign: follow-up monitoring, reassurance, and possible removal if causing discomfort.
If malignant: referral to an oncologist, staging tests, treatment planning, and a multidisciplinary team consultation.
What You MUST Do in the Next 48 Hours
Stop reading. Take action. Here's your immediate plan:
TODAY (Right Now)
1. Examine the Lump Again Properly
Note the exact location (describe in relation to anatomical landmarks). Note the size (compare to a pea, grape, marble, or walnut). Note the texture (hard as bone, firm, rubbery, or soft). Note the mobility (moves freely, slightly mobile, or completely fixed). Note any associated symptoms (pain, redness, discharge, skin changes). Write all of this down with today's date. Take a photograph with a ruler next to it for reference.
2. Book a Doctor Appointment
Do NOT wait for next month. Do NOT wait for it to "maybe go away."
Book for THIS WEEK. Not next month. THIS WEEK.
Options include your regular general practitioner, a breast specialist (for breast lumps), a urologist (for testicular lumps), or a surgical oncologist if you are very concerned.
When booking, say: "I've found a lump and need to be seen urgently." Most clinics will prioritize you.
3. Tell Someone Close
Your spouse, partner, parent, sibling, or close friend. Say: "I found a lump and I'm seeing a doctor this week. I wanted you to know."
Accountability matters. They will make sure you follow through.
4. Prepare Questions for Your Appointment
Write down:
"What do you think this lump might be?"
"What tests do you recommend?"
"How quickly do we need to act?"
"What are the next steps if it's concerning?"
"What should I watch for while waiting for test results?"
WITHIN 48 HOURS
5. Attend Your Appointment
Bring your written notes about the lump. Bring a list of any medications you take. Bring your medical history. Consider bringing someone with you for support and to help remember what is discussed.
6. Follow Through on Recommended Tests
If the doctor orders imaging or a biopsy, schedule it immediately. Do not leave the office without a confirmed appointment.
WHAT NOT TO DO
Do not spend hours googling symptoms — it will terrify you and provide unreliable information. Do not ask unqualified people for their opinion on your lump. Do not rely on home remedies or "wait and see." Do not convince yourself that "if it was serious, it would hurt." Do not cancel your appointment out of fear.
Professional Support Options
If you're experiencing possible cancer symptoms, seeking a second opinion, or unsure which tests or treatments are right for you, don't wait. Speak with a qualified oncologist today.
Connect with experienced U.S.-based cancer specialists for a comprehensive second-opinion consultation. They will carefully review your case and help determine the most appropriate next steps for your individual health needs:
👉 https://myamericandoctor.com/our-doctors/
You may also choose to enroll in our upcoming concierge medical clinic in India, Global Concierge Doctors. We offer U.S.-style primary care with 24/7 access to India-based physicians for ongoing guidance on any health concern. When required, we coordinate referrals to trusted specialists in India and the U.S. for advanced evaluation and care.
Your health decisions today shape your life tomorrow.
The Psychological Burden of "Not Knowing"
Here's something doctors don't often discuss: the mental health cost of denial.
The Anxiety Cycle
When you find a lump but don't get it checked, the psychological toll accumulates rapidly. In the first week, there is constant worry, repeated self-checking, difficulty concentrating at work, and lost sleep from late-night internet searches. By weeks two through four, the worry becomes a background presence — still there, but being actively suppressed. Sleep quality worsens. By months two to three, full-blown health anxiety can set in: every ache and unusual sensation is interpreted as spreading cancer, with panic attacks, low mood, and avoidance behaviours. By month four and beyond, the person is either in complete denial or struggling with a severe anxiety disorder that itself requires treatment.
The Relief of Knowing
Compare this to getting it checked promptly. You find the lump and schedule an appointment. Yes, you're anxious, but you're taking action. Tests are completed within a week or two. Results come back within days after that. If it's benign, there is immediate, massive relief. Anxiety disappears. You can move on with your life. If it's malignant, yes, that is difficult news — but at least you know. You can make a plan. You can take action. You can fight back. The uncertainty is over.
Psychological research consistently shows that uncertainty can be highly damaging to mental health, and that taking action and reducing uncertainty often reduces anxiety.
Special Considerations for Different Age Groups
Young Adults (18–35)
You might think you're "too young" for cancer. You're not.
Cancers that commonly affect young adults include testicular cancer (peak age 15–35), thyroid cancer, melanoma and skin cancers, lymphoma, breast cancer (yes, even in the 20s and 30s), and cervical cancer.
Your advantage: younger bodies often tolerate treatment better. Early detection is even more crucial because you have your whole life ahead of you.
Your challenge: doctors may occasionally underestimate risk due to age. Be persistent. Request the tests you need. Seek a second opinion if necessary.
Middle Age (35–55)
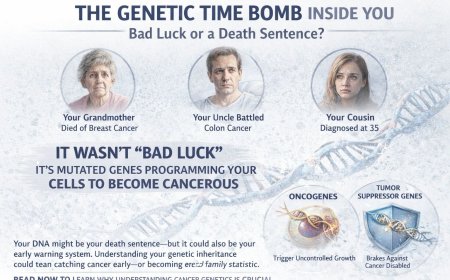
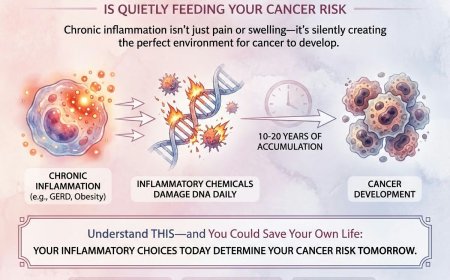
This is when cancer incidence begins rising significantly. Risk factors accumulate over time through genetic mutations, environmental exposure over decades, lifestyle factors such as diet and stress, and hormonal changes, particularly in women approaching menopause.
You can no longer rely on youth as a protective factor. Any new lump requires prompt evaluation. The good news is that people in this age group are often well-positioned in their careers and personal lives to prioritise their health.
Older Adults (55+)
Cancer incidence continues to rise with age, and most cancers occur in people over 55. Any new lump should be considered suspicious until proven otherwise. Do not dismiss symptoms as "just getting old." You likely have accumulated healthcare experience and possibly health insurance coverage — use it.
The Family Impact of Denial
When you delay getting a lump checked, it is not just about you.
If You're a Parent
Your children are watching how you handle health concerns. When you ignore a worrying symptom, you teach them that ignoring health problems is acceptable. You risk not being present for their major life milestones. You potentially burden them with late-stage cancer caregiving. And you model poor health decision-making.
When you address health concerns promptly, you demonstrate responsible self-care, show that asking for help is strength rather than weakness, maximise your chances of being there for their future, and set a meaningful example of proactive health management.
If You're a Spouse or Partner
Your partner's life is intertwined with yours. Late-stage cancer treatment can financially and emotionally devastate families. Your partner may need to become a full-time caregiver. Retirement plans, travel, time with grandchildren — all of it is at risk.
If You're the Primary Breadwinner
The implications extend beyond treatment. Lost income during months of treatment, possible disability or reduced ability to return to previous work, and compromised financial security for the family are all real consequences that can be avoided or significantly reduced through early detection.
Getting a lump checked isn't selfish. Ignoring it is.
Common Questions and Fears
"What if the biopsy hurts?"
Most biopsies are performed under local anaesthesia. You will feel pressure but minimal pain. The discomfort is brief and minor compared to the relief of knowing what you're dealing with.
"What if they find cancer?"
Then you'll deal with it — with knowledge, with a plan, and with modern medicine behind you. But right now, you don't know. And "not knowing" is causing you anxiety anyway.
"I can't afford the tests right now."
Early detection is always far less burdensome than late-stage treatment, both physically and in every other way. Look into government health schemes, NGO cancer screening programmes, hospital charity care programmes, and medical loans or payment plans. Many hospitals offer assistance — ask.
"I'm too busy at work."
You will not be able to work through months of intensive chemotherapy. A few hours for a doctor's appointment now is a fraction of the time late-stage treatment demands. The calculation is simple.
"My family needs me healthy; I can't be sick."
Ignoring a potential cancer will not keep you healthy. Your family needs you to be responsibly proactive about your health, not in denial.
"What if it's all in my head?"
Physical lumps are not psychological. If you can feel it, it is real. Even if it turns out to be entirely benign, you felt something real that deserves medical evaluation.
The Final Word: Your Lump's Message to You
If that lump could speak, here's what it would say:
"I'm here. You know I'm here. You've checked me seventeen times."
"I might be nothing. I might be something. But you won't know until you stop being scared and start being smart."
"Every day you ignore me is a day I could be growing. Spreading. Becoming harder to treat."
"Your life is in your hands. And you're holding me. What will you do?"
"Your children need you. Your spouse needs you. Your parents need you. You need you."
"I'm giving you a chance right now. A window of opportunity. Will you take it?"
"Or will you become another story of 'If only I'd gone to the doctor sooner'?"
Take Action NOW
Step 1: Put down your phone after reading this.
Step 2: Open your calendar and find the earliest available time this week.
Step 3: Call your doctor's office and book an appointment, saying "I've found a lump and need to be seen urgently."
Step 4: Tell someone you love about the lump — your spouse, parent, sibling, or best friend.
Step 5: Write down the details of your lump: location, size, texture, mobility, and how long you've noticed it.
Step 6: Screenshot this article to remind yourself why you're doing this.
Step 7: SHOW UP to your appointment. Don't cancel. Don't reschedule unless absolutely necessary.
Step 8: Follow through on any recommended tests immediately.
Your life is literally in your hands. And right now, you're holding a lump.
What happens next is YOUR choice.
Choose wisely. Choose quickly. Choose TODAY.
Share This Article
Know someone who found a lump and is making excuses not to get it checked? Know someone who keeps saying "It's probably nothing" despite having a persistent lump? Know someone who's terrified of doctors and avoiding what could be a life-saving appointment?
Share this article. It might save their life.
Every day of delay matters. Every week of denial counts. Every month of avoidance could be the difference between cure and catastrophe.
Be the friend who cares enough to share the truth, even when it's uncomfortable.
Reader Poll
Have you found a lump and not gotten it checked?
○ Yes, and after reading this I'm scheduling an appointment this week
○ Yes, and I've been avoiding it — but now I understand I need to act
○ No, I got any lumps checked immediately
○ No lumps currently, but I'll know what to do if I find one
Additional Resources
Cancer Screening Guidelines
Breast awareness / knowing what’s normal for you: ongoing, starting in early adulthood. If you notice a new lump, skin change, nipple change, or discharge, get evaluated promptly. Screening mammogram schedules vary by country and organization; many recommend that average-risk women begin screening in their 40s, with frequency based on age and risk. Follow your clinician’s advice and applicable national guidelines.
Testicular self-checks: guidance varies. Many clinicians recommend that men (especially ages 15–35) become familiar with what’s normal for them and seek medical care right away if they notice a new lump or change; some clinicians advise monthly self-checks.
Warning Signs to Never Ignore
Any new lump that persists for more than 2 weeks; lumps that are growing; lumps with associated skin changes; painful lumps that do not resolve; multiple lumps appearing simultaneously; and lumps with systemic symptoms such as fever, weight loss, or night sweats.
Emergency Situations Requiring Immediate Attention
Sudden severe swelling; a lump with severe pain and fever (possible infection or abscess); a lump that is rapidly growing; a lump with associated difficulty breathing or swallowing; and sudden severe testicular pain (possible testicular torsion).
A Message of Hope
While this article has been deliberately urgent and direct to motivate action, please know:
Most lumps are NOT cancer.
The majority of lumps evaluated by doctors turn out to be benign conditions — cysts, lipomas, swollen lymph nodes, fibroadenomas, and other harmless conditions.
But the ONLY way to know is through proper medical evaluation.
The goal of this article is not to terrify you. It is to overcome the inertia of denial and fear that prevents people from taking the simple step of seeing a doctor.
Early detection saves lives. It is that simple.
And if it IS cancer, catching it early often means less invasive treatment, better outcomes, faster recovery, higher cure rates, and far less disruption to your life and the lives of those who love you.
You deserve to know. You deserve to be treated. You deserve the best possible outcome.
Take the first step today.
Medical Disclaimer
This article is provided strictly for educational, informational, and awareness purposes only. It is not intended to be, and should not be construed as, professional medical advice, diagnosis, treatment, or a substitute for consultation with qualified healthcare professionals.
No Doctor-Patient Relationship
Reading this article does not establish a doctor-patient relationship between the reader and the author, publisher, or any affiliated entities. No medical decisions should be made based solely on the content of this article. Reading this article does not create any professional relationship, obligation, or responsibility between you and the author or publisher.
Consult Qualified Medical Professionals
If you have found a lump, noticed any concerning symptoms, masses, swelling, or any other physical changes mentioned in this article, seek immediate consultation with qualified oncologists, physicians, surgeons, or appropriate medical specialists. If you are experiencing severe symptoms — chest pain, difficulty breathing, severe pain, high fever, or any symptoms that concern you — contact emergency services or visit an emergency department immediately. This article is not a substitute for professional medical examination, diagnosis, and treatment.
Individual Medical Situations Vary
Every person's medical condition, health history, family history, genetic factors, risk factors, lifestyle factors, and circumstances are unique. Diagnostic tests, treatment options, surgical procedures, and medical recommendations must be tailored to individual patients through direct consultation with licensed healthcare providers who have access to complete medical histories, physical examination findings, and can perform proper clinical evaluations. What is appropriate for one person may not be appropriate for another.
Not a Recommendation for Specific Tests or Treatments
References to mammograms, ultrasounds, biopsies, fine needle aspiration, core needle biopsy, excisional biopsy, CT scans, MRI scans, surgical procedures, chemotherapy, radiation therapy, or any other diagnostic procedures or treatments in this article are for informational and educational purposes only. These references do not constitute recommendations that you should or should not undergo these tests or treatments. All decisions regarding medical testing, diagnosis, surgical interventions, and treatment should be made in consultation with qualified healthcare professionals based on your specific medical situation, risk factors, and clinical presentation.
No Guarantee of Accuracy or Completeness
While efforts have been made to provide accurate and current information, medical knowledge, research findings, clinical guidelines, diagnostic techniques, treatment protocols, and medical practices continuously evolve. The information in this article may not reflect the most current research, clinical guidelines, treatment options, or medical practices. The author and publisher make no representations or warranties regarding the accuracy, completeness, currency, or timeliness of the content. Medical information can become outdated quickly, and this article may not reflect recent developments in cancer detection, diagnosis, or treatment.
No Guarantees of Outcomes
No article can guarantee specific medical outcomes. Cancer detection, diagnosis, prognosis, treatment success, survival rates, and patient experiences vary tremendously based on countless individual factors including cancer type, stage at detection, grade, molecular characteristics, patient age, overall health, response to treatment, access to care, and many other variables. Statistics, survival rates, and outcome data presented in this article represent general population averages and may not apply to individual cases.
Do Not Disregard or Delay Professional Medical Advice
Never disregard, avoid, or delay obtaining professional medical advice from qualified healthcare providers because of something you have read in this article. If you have questions or concerns about information presented here, or if you have symptoms that concern you, discuss them immediately with your personal physician, oncologist, surgeon, or appropriate medical specialist. Delaying appropriate medical care can have serious consequences. This article should motivate you to seek professional care, not replace it.
Not a Substitute for Professional Mental Health Care
If you are experiencing significant anxiety, depression, panic attacks, or other mental health concerns related to health fears or a cancer diagnosis, please seek care from qualified mental health professionals including psychologists, psychiatrists, licensed counselors, or therapists who specialise in medical trauma and health anxiety.
Third-Party Resources and Links
Any references to third-party medical services, clinics, doctors, hospitals, diagnostic centers, online second-opinion services, external websites, or other resources are provided for informational purposes only and do not constitute endorsements, recommendations, or guarantees of quality or appropriateness. The author and publisher are not responsible for the content, services, qualifications, or practices of any third-party entities; do not verify the credentials, competence, or quality of third-party providers; make no representations about the suitability of any third-party services for your specific needs; and are not responsible for any outcomes, complications, or consequences resulting from use of third-party services. You are responsible for conducting your own due diligence, verifying credentials, checking references, and making informed decisions about any healthcare providers or services.
Patient Stories and Case Studies
Any patient stories, case studies, scenarios, or examples included in this article are used for illustrative and educational purposes only. They may be fictionalized, composite cases, or generalised examples. They do not represent specific real individuals and should not be interpreted as typical outcomes. Your experience and medical situation will be unique. Do not compare your situation to examples in this article or expect similar outcomes.
Limitation of Liability
To the fullest extent permitted by law, the author, publisher, affiliated entities, employees, agents, and representatives disclaim all liability for any direct, indirect, incidental, consequential, special, exemplary, or punitive damages arising from the use of, reliance on, or inability to use information contained in this article. This includes but is not limited to: medical complications or adverse outcomes; delayed diagnosis due to misunderstanding of information; emotional distress or psychological harm; missed opportunities for earlier diagnosis or treatment; and any other adverse outcomes related to health or wellbeing. By using this information, you agree to hold harmless the author, publisher, and all affiliated parties from any claims related to your use of this information.
Geographic and Regulatory Considerations
Medical regulations, standards of care, insurance coverage, healthcare system structures, availability of diagnostic tests, treatment protocols, licensing requirements for healthcare providers, and legal frameworks vary significantly by country, state, region, and healthcare setting. Information regarding procedures, tests, treatments, timelines, and medical practices may not be applicable to all geographic locations or healthcare settings. Healthcare policies and available resources in India may differ substantially from other countries, and resources vary within India across different states and between urban and rural areas. Always verify what services, tests, and treatments are available and appropriate in your specific location.
No Legal or Financial Advice
This article does not provide legal advice regarding medical decision-making, malpractice, patient rights, insurance claims, disability claims, or any other legal matters. It does not provide financial advice regarding insurance selection, medical financing, or any other financial matters. Consult appropriate legal and financial professionals for such advice.
Your Responsibility and Informed Decision-Making
You acknowledge and agree that you are solely responsible for your own health decisions and outcomes; that you will consult with appropriate licensed healthcare professionals before making any medical decisions; that you will undergo proper clinical evaluation before making any decisions regarding diagnostic tests or treatments; that you understand this article is not personalised to your specific situation; that you will not rely solely on this article for medical decision-making; and that you will exercise your own independent judgment in all medical matters.
Acknowledgment
By reading and using the information in this article, you acknowledge that you have read, understood, and agreed to this disclaimer in its entirety. You further acknowledge that this article has been created with the assistance of artificial intelligence. While every effort has been made to ensure accuracy, AI-generated content may occasionally contain errors, omissions, or inaccuracies. The information presented here is intended solely for educational and informational purposes and should not be relied upon as a substitute for professional medical advice. Readers are strongly encouraged to consult qualified healthcare professionals, refer to peer-reviewed medical literature, and cross-reference information from established clinical sources before making any health-related decisions.
Remember: This article is a tool to motivate action, not to replace professional medical care. Its purpose is to overcome denial and encourage prompt medical evaluation. Always consult qualified healthcare professionals for actual medical advice, diagnosis, and treatment.
Last Updated: February 3, 2026
What's Your Reaction?
 Like
0
Like
0
 Dislike
0
Dislike
0
 Love
0
Love
0
 Funny
0
Funny
0
 Angry
0
Angry
0
 Sad
0
Sad
0
 Wow
0
Wow
0