The PSA Dilemma: What Your Doctor May Not Be Telling You About Prostate Cancer Screening
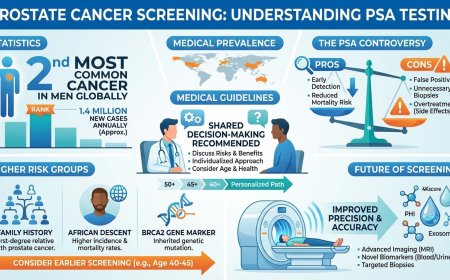
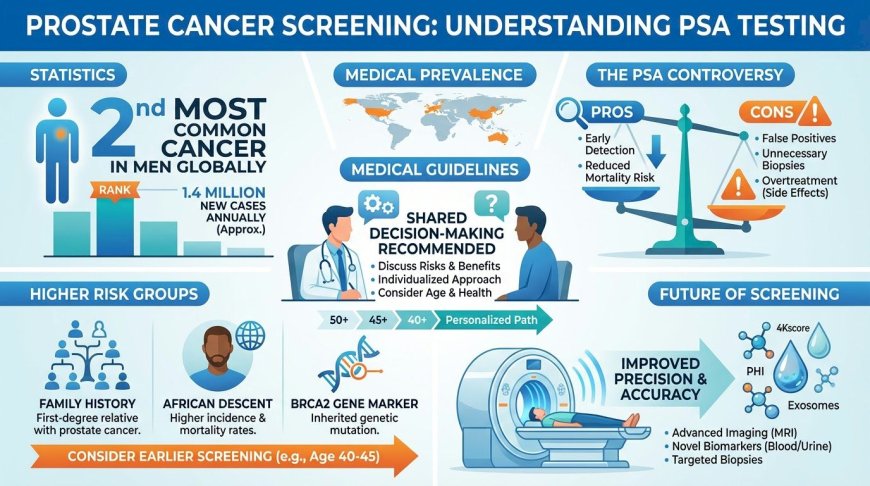
Prostate cancer is the second most common cancer in men globally, yet its primary screening tool — the PSA blood test — remains deeply controversial. While PSA testing can detect cancer early and reduce mortality, it is not cancer-specific, frequently producing false positives that trigger unnecessary biopsies and overtreatment. Major medical bodies disagree on screening guidelines, but universally recommend shared decision-making between patient and doctor. Higher-risk men — those with family history, of African descent, or carrying BRCA2 mutations — should consider earlier screening. Emerging technologies like MRI-guided biopsies and advanced biomarkers are improving precision and gradually shifting the benefit-harm balance toward screening.
At A Glance
You are 52 years old. Your annual check-up is approaching. You have heard about the PSA test — a blood test used in the detection of prostate cancer. You are unsure whether you should ask for it, whether you truly need it, or whether undergoing the test could lead to anxiety, further testing, or treatment that may not ultimately benefit you. Your doctor, too, may appear cautious or noncommittal.
This uncertainty is not accidental.
Prostate cancer is the second most commonly diagnosed cancer in men worldwide and among the leading causes of cancer-related death in men globally. In India, its incidence has been rising steadily, particularly in urban populations. Despite this, there remains no universal agreement within the medical community on whether routine screening using PSA should be recommended for all men, or how best to implement it.
This article examines the scientific, clinical, and ethical debate surrounding prostate cancer screening — not to alarm you, but to equip you with the knowledge required to participate meaningfully in an informed discussion with your physician.
What Is PSA and Why Is It Controversial?
PSA, or Prostate-Specific Antigen, is a protein produced by prostate tissue and measurable through a blood test. Elevated PSA levels may be associated with prostate cancer, but they are not exclusive to it.
PSA levels can rise due to several non-cancerous conditions, including benign prostatic hyperplasia (BPH), prostatitis, urinary tract infections, recent ejaculation, and even physical activity affecting the prostate. Conversely, some men with prostate cancer may have PSA values within the traditionally accepted “normal” range.
This lack of cancer specificity means PSA testing can lead to false-positive results, unnecessary biopsies, psychological distress, and detection of slow-growing cancers that might never cause symptoms during a man’s lifetime. At the same time, reliance on PSA alone may fail to identify some clinically significant cancers.
This balance between potential benefit and harm is the core reason PSA screening has remained controversial for more than three decades.
The Numbers That Require Careful Interpretation
Large population studies illustrate both the benefits and the limitations of PSA screening.
Modeling studies examining cohorts of men in their 50s who undergo PSA-based screening show that a proportion will receive positive results, fewer will undergo biopsy, and an even smaller number will ultimately avoid death from prostate cancer due to early detection. At the same time, a significant number of men may be diagnosed with prostate cancers that would never have caused symptoms or shortened life expectancy.
Long-term follow-up data from the European Randomized Study of Screening for Prostate Cancer (ERSPC) demonstrate a modest reduction in prostate cancer–specific mortality associated with screening. However, the absolute number of men who need to be screened to prevent one prostate cancer death remains high, highlighting the importance of individualized risk assessment rather than universal testing.
These data underscore that PSA screening offers potential benefit for some men while exposing others to avoidable harm.
What Major Guidelines Say — And Why They Differ
Conflicting recommendations reflect genuine scientific disagreement rather than confusion or negligence.
United States Preventive Services Task Force (USPSTF):
Recommends individualized decision-making for men aged 55–69 after discussion of potential benefits and harms. Recommends against routine PSA screening in men aged 70 and older.
American Cancer Society (ACS):
Recommends informed discussion about screening beginning at age 50 for average-risk men, age 45 for men at higher risk (including those with a first-degree relative diagnosed before age 65), and age 40 for men at very high risk. ACS does not recommend routine prostate self-examinations as a screening tool.
European Association of Urology (EAU) – 2024 Guidelines:
Recommends that PSA testing should not be performed without prior counseling. Suggests consideration of screening in informed men at increased risk, including those with family history, men of African ancestry, and carriers of BRCA2 mutations.
UK National Screening Committee (Draft Position, Late 2025):
Issued a draft recommendation against routine PSA screening, including for higher-risk groups, citing concerns over overdiagnosis and overtreatment. This position remains debated among specialists.
National Comprehensive Cancer Network (NCCN):
Supports baseline PSA testing from age 45 with risk-adapted follow-up strategies.
Despite differences, nearly all guidelines emphasize shared decision-making as essential.
Overdiagnosis Versus Missed Disease
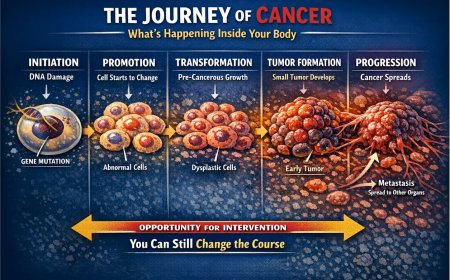
Prostate cancer presents a unique challenge: many detected tumors are biologically indolent and may never threaten health or longevity.
Population-based registry studies indicate that many men diagnosed with localized prostate cancer are more likely to die from unrelated causes than from prostate cancer itself. This reality has led to increasing adoption of active surveillance strategies for low-risk disease.
However, aggressive prostate cancer does exist. When diagnosed at an advanced or metastatic stage, it is not curable. Delayed diagnosis may result in significantly worse outcomes.
The challenge is distinguishing early between cancers that require intervention and those that do not — a distinction that PSA alone cannot reliably make.
Advances That Are Changing the Screening Pathway
Technological developments are helping address earlier limitations of PSA-based screening.
Multi-parametric MRI (mpMRI) allows noninvasive visualization of suspicious prostate lesions before biopsy. MRI-targeted biopsies improve detection of clinically significant cancers while reducing unnecessary sampling.
Biomarker-based tests such as the Prostate Health Index (PHI) and kallikrein-based panels are increasingly used to refine risk assessment following elevated PSA results. Urine- and blood-based molecular assays are under active investigation and may further improve precision.
These advances support a shift toward risk-adapted, stepwise screening strategies rather than blanket testing.
Illustrative Patient Scenario
A 58-year-old man undergoes PSA testing and receives a mildly elevated result. Subsequent evaluation identifies low-grade, organ-confined prostate cancer. He undergoes definitive treatment and later experiences lasting urinary and sexual side effects.
Years later, he learns that active surveillance would now be considered an appropriate, guideline-supported option for his cancer profile.
This scenario reflects a commonly observed clinical pattern and highlights the importance of informed counseling rather than reflexive treatment decisions.
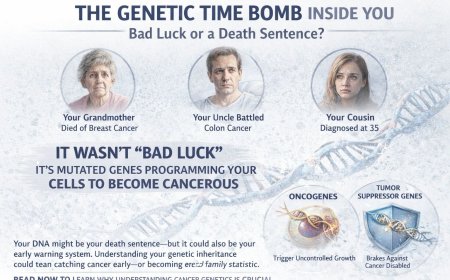
Who May Benefit More From Screening?
Certain factors increase prostate cancer risk:
-
Increasing age
-
Family history in first-degree relatives
-
African ancestry
-
Known hereditary cancer mutations such as BRCA2
Men with these risk factors may benefit from earlier or more vigilant discussions about screening.
The Shared Decision-Making Conversation
Before undergoing PSA testing, men should discuss:
-
Individual risk factors
-
Potential benefits and harms
-
Possible downstream testing pathways
-
The role of MRI and surveillance
-
Personal values regarding quality of life and uncertainty
There is no universally correct choice — only an informed one.
Key Takeaways
PSA screening can reduce prostate cancer mortality for some men but carries real risks of overdiagnosis and overtreatment. Advances in imaging and biomarkers are improving the balance of benefit and harm, but shared decision-making remains central to responsible care.
Professional Support Options
If you're experiencing possible cancer symptoms, seeking a second opinion, or unsure which tests or treatments are right for you, don't wait. Speak with a qualified oncologist today.
Connect with experienced U.S.-based cancer specialists for a comprehensive second-opinion consultation. They will carefully review your case and help determine the most appropriate next steps for your individual health needs:
👉 https://myamericandoctor.com/our-doctors/
You may also choose to enroll in our upcoming concierge medical clinic in India, Global Concierge Doctors. We offer U.S.-style primary care with 24/7 access to India-based physicians for ongoing guidance on any health concern. When required, we coordinate referrals to trusted specialists in India and the U.S. for advanced evaluation and care.
Your health decisions today shape your life tomorrow.
Medical Disclaimer
This article is provided strictly for educational, informational, and awareness purposes only. The real-life patient stories and examples shared in this article are drawn from clinical experiences, patient interactions, and commonly observed scenarios in oncology practice. They are presented for educational and awareness purposes only. Names and identifying details have been changed to protect patient privacy. While these accounts reflect authentic experiences encountered in medical practice, they have not been independently documented or published by us as formal case studies. Individual experiences with cancer diagnosis, treatment, and outcomes vary widely, and no single story should be taken as representative of what any reader may experience. It is not intended to be, and should not be construed as, professional medical advice, diagnosis, treatment, or a substitute for consultation with qualified healthcare professionals.
No Doctor-Patient Relationship
The information presented in this article does not establish a doctor-patient relationship between the reader and the author, publisher, or any affiliated entities. No medical decisions should be made based solely on the content of this article.
Consult Qualified Medical Professionals
If you are experiencing any urinary symptoms, have received an elevated PSA result, have been diagnosed with prostate cancer, or have concerns about prostate cancer risk, seek immediate consultation with qualified oncologists, urologists, or appropriate medical specialists. For medical emergencies, contact emergency services immediately.
Individual Medical Situations Vary
Every person's medical condition, health history, risk factors, cancer type, and circumstances are unique. Diagnostic tests, treatment options, and medical recommendations must be tailored to individual patients through direct consultation with licensed healthcare providers who have access to complete medical histories and can perform proper clinical evaluations.
Not a Recommendation for Specific Tests or Treatments
References to PSA testing, biopsies, MRI, CT scans, PET scans, blood tests, tumor markers, chemotherapy, radiation therapy, immunotherapy, targeted therapy, surgery, active surveillance, or any other diagnostic procedures and treatments in this article are for informational purposes only and do not constitute recommendations that you should or should not undergo these tests or treatments. All decisions regarding medical testing, diagnosis, and treatment should be made in consultation with qualified healthcare professionals based on your specific medical situation.
No Guarantee of Accuracy or Completeness
While efforts have been made to provide accurate information, medical knowledge continuously evolves, particularly in the rapidly advancing field of oncology. The information in this article may not reflect the most current research, clinical guidelines, treatment protocols, or medical practices. The author and publisher make no representations or warranties regarding the accuracy, completeness, or timeliness of the content.
Do Not Disregard or Delay Professional Medical Advice
Never disregard, avoid, or delay obtaining professional medical advice from qualified healthcare providers because of something you have read in this article. If you have questions or concerns about information presented here, discuss them with your personal physician or urologist. Early detection and prompt treatment significantly improve cancer outcomes.
Third-Party Resources and Links
Any references to third-party medical services, clinics, doctors, cancer centers, or external websites are provided for informational purposes only and do not constitute endorsements. The author and publisher are not responsible for the content, services, or practices of any third-party entities.
Limitation of Liability
To the fullest extent permitted by law, the author, publisher, and affiliated entities disclaim all liability for any direct, indirect, incidental, consequential, or punitive damages arising from the use of, or reliance on, information contained in this article. This includes, but is not limited to, medical complications, treatment decisions, or any other adverse outcomes.
Geographic and Regulatory Considerations
Medical regulations, standards of care, insurance coverage, availability of diagnostic tests, treatment protocols, and access to cancer therapies vary by country, region, and healthcare system. Information regarding procedures and medical practices may not be applicable to all geographic locations or healthcare settings.
Clinical Trials and Experimental Treatments
Any references to clinical trials, experimental treatments, or investigational therapies are for informational purposes only. Participation in clinical trials should only be considered after thorough discussion with your oncology team and understanding of all risks and benefits.
Your Responsibility
You acknowledge that you are solely responsible for your own health decisions and that you will consult with appropriate licensed healthcare professionals before making any medical decisions or undergoing any diagnostic tests or treatments.
Acknowledgment
By reading and using the information in this article, you acknowledge that you have read, understood, and agreed to this disclaimer in its entirety. You further acknowledge that this article has been created with the assistance of artificial intelligence. While every effort has been made to ensure accuracy, AI-generated content may occasionally contain errors, omissions, or inaccuracies. The information presented here is intended solely for educational and informational purposes and should not be relied upon as a substitute for professional medical advice. Readers are strongly encouraged to consult qualified healthcare professionals, refer to peer-reviewed medical literature, and cross-reference information from established clinical sources before making any health-related decisions.
Last Updated: February 2026
What's Your Reaction?
 Like
0
Like
0
 Dislike
0
Dislike
0
 Love
0
Love
0
 Funny
0
Funny
0
 Angry
0
Angry
0
 Sad
0
Sad
0
 Wow
0
Wow
0