Cardiac Amyloidosis - The Silent Protein Invasion: Why Your "Normal" Heart Tests Might Be Missing a Deadly Disease
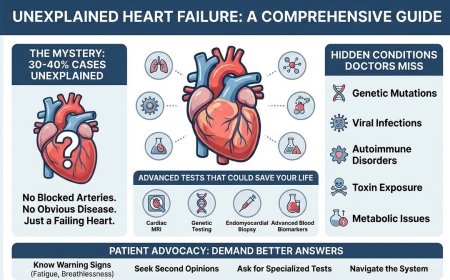
Cardiac amyloidosis is a progressive, often misdiagnosed heart condition where abnormal proteins accumulate in the heart muscle, causing heart failure and potentially fatal complications. Despite affecting 13-17% of heart failure patients, it remains undetected because standard cardiac tests miss it. This comprehensive guide reveals the warning signs doctors often overlook—from unexplained heart failure with preserved ejection fraction to the surprising connection with carpal tunnel syndrome. Learn about the life-saving cardiac amyloid scan (Tc99m-PYP), understand the difference between ATTR and AL types, discover new treatments like tafamidis and acoramidis that can add years to your life, and find out if you need testing before it's too late.
Your echocardiogram came back fine. Your ECG looks normal. Your stress test? Passed with flying colors.
Your cardiologist says, "Everything looks good."
But you're still exhausted. Still breathless. Your legs are swelling. Your heart feels... heavy.
"Maybe it's just age," you tell yourself.
Here's what no one is telling you: A deadly protein could be strangling your heart RIGHT NOW, and your standard tests can't see it.
The Disease Hiding in Plain Sight
Right now, thousands of Indians are possibly walking around with cardiac amyloidosis - a progressive, deadly heart condition that's being dismissed as "normal aging," "heart failure," or "stiff heart syndrome."
They've seen multiple doctors. Had dozens of tests. Been told their hearts are "just getting old."
They're dying slowly because no one thought to do ONE specific scan or is not available locally.
The cardiac amyloid scan.
Sound familiar? Here's why you should be concerned:
- You're over 60 with unexplained heart failure
- Your heart walls are thickened but doctors can't explain why
- You're exhausted all the time despite "normal" test results
- You have prior history of carpal tunnel syndrome
- You have an irregular heartbeat that doesn't respond well to treatment
- Your doctor used words like "restrictive cardiomyopathy" or "diastolic dysfunction"
If ANY of these apply to you, keep reading. Your life might depend on it.
What Your Cardiologist Isn't Telling You (Because They Might Not Know)
Here's the terrifying truth about cardiac amyloidosis:
It's far more common than anyone realized.
For decades, it was considered a "rare disease." Recent studies have shattered that myth:
- 13-17% of patients with heart failure with preserved ejection fraction (HFpEF) have cardiac amyloidosis
- Up to 16% of elderly patients with severe aortic valve stenosis have it
- Many patients labeled with "hypertensive heart disease" actually have amyloidosis
That's not rare. That's an epidemic hiding in plain sight.
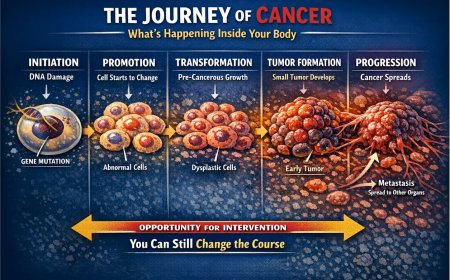
The disease works like this:
Abnormal proteins (amyloid) build up in your heart muscle. Slowly. Silently. These proteins are like concrete filling the walls of your heart, making it stiff and unable to pump effectively.
Your heart becomes rigid. It can't relax properly between beats. It can't fill with blood. It struggles to pump.
And it gets worse. Every. Single. Day.
The Journey of Misdiagnosis: A Story That Could Be Yours
Meet Suresh, 68, retired bank manager from Mumbai.
Year 1: Shortness of breath climbing stairs. "You're just out of shape," his doctor said.
Year 2: Severe fatigue. Swelling in ankles. Echo showed "thickened heart walls." Diagnosed with hypertensive heart disease. Started on heart failure medications.
Year 3: Symptoms worsening despite treatment. Developed carpal tunnel syndrome in both hands. "Coincidence," they said.
Year 4: More tests. More medications. Nothing helping. Lost 15kg because he felt too tired to eat. Started using a walking stick.
Year 5: A new cardiologist looked at his constellation of symptoms and said five words that changed everything:
"Has anyone done an amyloid scan?"
The scan took 3 hours. The diagnosis took 5 days.
Cardiac amyloidosis. Had been there all along.
Five years of suffering. Five years of wrong treatment. Five years of irreversible heart damage - all because no one thought to do a single scan.
Suresh cried when he got the diagnosis. Not because it was bad news (though it was). But because finally, after five years, someone had found the REAL answer.
The Cruel Mathematics of Late Diagnosis
Let me show you numbers that should genuinely terrify you:
If diagnosed early (when symptoms first appear):
- Median survival with treatment: 4-5 years or more
- Quality of life: Manageable with proper treatment
- Treatment options: Multiple medications now available
If diagnosed late (after years of misdiagnosis):
- Median survival: 6-12 months
- Quality of life: Severely compromised
- Treatment options: Limited effectiveness due to advanced damage
Do you see the problem?
Every month of delay isn't just wasted time. It's lost survival time. It's irreversible heart damage. It's your life slipping away.
And standard cardiac tests can't detect it until it's advanced.
Why Standard Heart Tests Miss Cardiac Amyloidosis
Your cardiologist orders the usual tests:
Echocardiogram: Shows thickened heart walls. But so do many conditions. Amyloidosis creates a specific "sparkling" pattern in the heart muscle, but many technicians and doctors miss it or mistake it for normal aging.
ECG: Shows low voltage despite thickened heart walls - a suspicious combination. But this "red flag" gets ignored or explained away.
Blood tests: BNP or NT-proBNP might be elevated. But these are elevated in ALL heart failure cases. Not specific enough.
Stress test: Might show reduced exercise capacity. But again - not specific.
Even cardiac MRI might show some concerning patterns, but amyloidosis requires specific imaging sequences that aren't always included in standard protocols.
Here's the brutal truth:
Cardiac amyloidosis is the master of disguise. It mimics other heart conditions perfectly. Unless your doctor specifically LOOKS for it with the RIGHT test, they'll miss it.
The ONE Scan That Changes Everything
The cardiac amyloid scan (technically called Tc99m-PYP scan or Tc99m-DPD scan) is a nuclear medicine imaging test that can detect amyloid deposits in your heart with remarkable accuracy.
How it works:
- A radioactive tracer is injected into your vein
- This tracer specifically binds to certain types of amyloid protein (ATTR amyloidosis)
- After 1-3 hours, you undergo imaging
- If amyloid is present in your heart, the scan will "light up" showing exactly where the protein has accumulated
The accuracy is stunning:
- Sensitivity: 97-100% for ATTR cardiac amyloidosis
- Specificity: 86-100%
Translation: If you have ATTR amyloidosis, this scan will almost certainly catch it.
The Two Types of Cardiac Amyloidosis (And Why It Matters)
There are two main types that affect the heart:
AL Amyloidosis (Light Chain)
- Caused by abnormal antibody proteins from bone marrow
- More aggressive, progresses faster
- Requires different testing (bone marrow biopsy, special blood tests)
- Median survival without treatment: 6 months
- Treated by hematologists with chemotherapy-like drugs
ATTR Amyloidosis (Transthyretin)
- Caused by misfolded transthyretin protein from liver
- Two subtypes:
- Wild-type (ATTRwt): Age-related, typically affects men over 60
- Hereditary (ATTRv): Genetic mutation, can affect younger patients
The cardiac amyloid scan detects ATTR amyloidosis. If positive, you can often avoid a heart biopsy - the scan alone is diagnostic in the right clinical context.
For AL amyloidosis, you need additional blood tests and possibly a bone marrow biopsy.
Why this matters to you:
The treatment is COMPLETELY different for each type. Getting the type wrong means getting the treatment wrong. Getting the treatment wrong means... well, you don't survive.
The Warning Signs Your Doctor Might Be Missing
Cardiac amyloidosis often comes with a constellation of symptoms and findings. The more of these you have, the higher your suspicion should be:
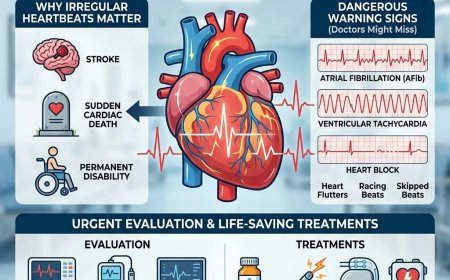
Cardiac Red Flags:
- Heart failure with preserved ejection fraction (your "pump function" looks normal, but you still have heart failure)
- Thickened heart walls WITHOUT a history of high blood pressure
- Low ECG voltage despite thick heart walls on echo
- Atrial fibrillation (irregular heartbeat) that's difficult to control
- Intolerance to standard heart failure medications (you feel worse on them, not better)
Non-Cardiac Clues (These Are CRITICAL):
- Carpal tunnel syndrome (especially bilateral - both hands)
- Lumbar spinal stenosis requiring surgery
- Biceps tendon rupture (happened spontaneously or with minor trauma)
- Peripheral neuropathy (numbness, tingling in feet and hands)
- Unexplained weight loss
- Autonomic dysfunction (dizziness when standing, digestive issues, bladder problems)
Family History Alerts:
- Multiple family members with "heart failure" at relatively young ages
- Family history of "familial amyloidosis"
- Ancestry from certain regions (Portugal, Sweden, Japan have higher rates of hereditary forms)
If you have heart symptoms PLUS any of these non-cardiac findings, you need to DEMAND an amyloid workup.
The Life-or-Death Difference: A Real Comparison
Patient A: Standard treatment for "heart failure"
- Medications that don't help much
- Symptoms progressively worsen
- Multiple hospitalizations
- Survival: 2-3 years from symptom onset
- Quality of life: Poor, declining rapidly
Patient B: Diagnosed with cardiac amyloid scan, proper treatment started
- Specific medications that actually work (tafamidis or acoramidis for ATTR, chemotherapy-like drugs for AL)
- Symptoms stabilize or improve slightly
- Fewer hospitalizations
- Survival: 4-6+ years with better quality of life
- Quality of life: Manageable, some patients maintain independence
The only difference? One scan. One correct diagnosis.
What Actually Happens During the Scan
Let me walk you through it so you know what to expect:
Day 1 - Injection:
- You arrive at the nuclear medicine department
- A small amount of radioactive tracer is injected through an IV (takes 2 minutes)
- You wait 1-3 hours for the tracer to circulate and bind to any amyloid
- During this time, you can sit comfortably, read, or even leave and return
Day 1 - Imaging:
- You lie on a table while a special camera takes images of your chest
- The camera doesn't touch you - it just detects the radiation from the tracer
- Takes 15-30 minutes
- Completely painless
- No claustrophobia (unlike MRI)
Day 2 or 3 - Second Imaging:
- You return for delayed images (usually 24-72 hours later)
- No new injection needed
- Same process - lie down, get imaged
- This delayed imaging helps distinguish heart uptake from blood pool
Results:
- Visual score (0-3) based on how much tracer accumulated in your heart
- Score of 2 or 3 = highly suspicious for ATTR amyloidosis
- Report typically ready in 2-3 days
The radiation exposure?
About the same as a regular nuclear stress test or a few months of natural background radiation. The benefits of diagnosis FAR outweigh the minimal radiation risk.
The Three Deadly Mistakes Patients Make
Mistake #1: "I'll Wait Until My Symptoms Get Worse"
The Brutal Reality: With cardiac amyloidosis, by the time your symptoms get significantly worse, the damage is often irreversible. The disease doesn't wait for you to be "ready" to get diagnosed.
Every month you wait is a month of:
- Additional protein deposits in your heart
- Progressive heart stiffening
- Reduced treatment effectiveness
- Lower survival probability
If you have unexplained heart failure with ANY of the red flags mentioned - discuss getting the scan NOW, not "when things get worse."
Mistake #2: "My Echo Was Normal, So I'm Fine"
The Brutal Reality: An echo can look "relatively normal" early in the disease. Or the findings can be misinterpreted as "just aging" or "hypertensive heart disease."
Classic echo findings that suggest amyloidosis:
- Increased wall thickness with "sparkling" or granular appearance
- Biatrial enlargement (both upper chambers enlarged)
- Small pericardial effusion (fluid around heart)
- Restrictive filling pattern
- "Apical sparing" on strain imaging (a specific pattern)
Most general cardiologists aren't looking for these subtle signs. If your symptoms don't match your echo findings, push for further testing.
Mistake #3: "The Scan Is Too Expensive/Unnecessary"
The Brutal Reality:
Cost of amyloid scan in India: ₹15,000 - 30,000 (please contact your local clinic for accurate cost)
Cost of years of wrong treatment:
- Wrong medications: ₹20,000 - 50,000 per year
- Multiple hospitalizations: ₹1,00,000 - 3,00,000 per event
- Advanced heart failure treatment: ₹5,00,000 - 20,00,000+
- Lost years of life: Priceless
Cost of proper treatment after correct diagnosis:
- Yes, treatment is expensive (tafamidis costs ₹10-12 lakhs per year)
- But you're treating the RIGHT disease
- You have a chance at stability and added years
- Some treatments have assistance programs
Which scenario costs more? Wrong treatment for 5 years, or correct diagnosis and appropriate therapy?
Who Needs This Scan? (Could Be You)
You should strongly consider a cardiac amyloid scan if you have:
High Priority (Scan Strongly Recommended):
- Heart failure with preserved ejection fraction (HFpEF) AND age >60
- Unexplained heart failure with thickened heart walls
- Heart failure + bilateral carpal tunnel syndrome
- Heart failure + low ECG voltage despite thick heart walls
- Heart failure + peripheral neuropathy
- Severe aortic stenosis needing valve replacement
Medium Priority (Discuss with Your Cardiologist):
- Heart failure that doesn't respond well to standard medications
- Heart failure + family history of amyloidosis
- Heart failure + unexplained weight loss
- Atrial fibrillation that's hard to control + other red flags
Consider Screening:
- Strong family history of amyloidosis (hereditary forms)
- Ancestry from high-risk populations
- Men over 70 with any heart failure symptoms
The Questions You MUST Ask Your Cardiologist
Don't just accept "heart failure" as your final diagnosis. Push for answers:
1. "Could this be cardiac amyloidosis?"
If they dismiss it immediately without considering your symptoms, that's a red flag. Any good cardiologist will at least consider it if you have the right clinical picture.
2. "Do I have any red flags for amyloidosis?"
- Low voltage ECG with thick walls?
- Carpal tunnel or other extra-cardiac manifestations?
- Restrictive physiology on echo?
3. "Should I get a cardiac amyloid scan?"
Be direct. If they say no, ask why not. Make them explain their reasoning.
4. "What's my ejection fraction and filling pattern?"
Preserved ejection fraction (>50%) with diastolic dysfunction may suggest cardiac amyloidosis.
5. "Have you seen cardiac amyloidosis patients before?"
Not all cardiologists have experience with this. If they haven't, consider getting a second opinion at a center with amyloidosis expertise.
Remember: You are your own best advocate. If something doesn't feel right, push for answers.
The Treatment Revolution (Why Diagnosis Now Matters More Than Ever)
Here's the GOOD news that makes getting diagnosed NOW so crucial:
For the first time in history, we have effective treatments for cardiac amyloidosis.
For ATTR Amyloidosis:
Tafamidis (Vyndaqel/Vyndamax) and Acoramidis (Attruby):
- FDA/EMA approved
- Stabilizes the TTR protein, prevents it from misfolding
- Reduces mortality by 30%
- Reduces hospitalizations by 32%
- Slows disease progression significantly
- Game-changer drug
Other emerging treatments:
- Patisiran and inotersen (for hereditary forms with neuropathy)
- AG10 (investigational, shows promise)
- Gene silencing therapies (cutting-edge)
For AL Amyloidosis:
Chemotherapy-based regimens:
- Target the abnormal plasma cells producing amyloid
- Aim to eliminate the source of amyloid production
- Can lead to significant organ improvement if caught early
Autologous stem cell transplant:
- For eligible patients
- Can be curative in some cases
The critical point:
All these treatments work BEST when started EARLY. Once your heart is severely damaged, even the best medications can't turn back the clock.
This is why that scan - that one diagnostic test - is so crucial. It opens the door to treatments that can add YEARS to your life.
The Difference Between Being Diagnosed Now vs. Later
Let me paint two very different futures for you:
Future A: You Get Diagnosed NOW
Year 1 after diagnosis:
- Start appropriate treatment (tafamidis for ATTR or chemotherapy for AL)
- Symptoms stabilize
- You can still walk, work, live relatively normally
- Regular monitoring shows disease is not progressing rapidly
Year 2-3:
- Treatment continues
- You've adjusted to your new medications
- Your heart function hasn't deteriorated significantly
- You're there for your daughter's wedding
- You meet your first grandchild
Year 4-5+:
- Still stable on treatment
- Quality of life is reasonable
- You've gained precious time with family
- New treatments emerge that you're eligible for
- You had YEARS that would have been lost
Future B: Diagnosis Comes Too Late
Year 1-2 (undiagnosed):
- Multiple doctor visits with no answers
- Symptoms getting worse
- Wrong treatments making you feel worse
- Frustration and despair
Year 3 (finally diagnosed):
- Cardiac amyloidosis confirmed
- But extensive heart damage already done
- Heart function severely impaired
- Treatment started but limited effectiveness
Year 4:
- Despite treatment, rapid decline
- Multiple hospitalizations
- Can barely walk across a room
- Considering heart transplant but may not be eligible
- Saying goodbyes you didn't expect to say so soon
Year 5:
- Hospice care
- Family gathered around
- Wondering "what if we'd found this earlier?"
Which future do you want?
The scan determines which path you're on.
The Brutal Truth About "Watching and Waiting"
I know what you're thinking:
"Maybe I'll just wait and see how I feel. If I get worse, then I'll get the scan."
Here's why that's a fatal mistake:
Cardiac amyloidosis doesn't pause. It doesn't plateau. It progresses.
Every month you "watch and wait" is a month of:
- More amyloid deposition
- More heart stiffening
- More irreversible damage
- Reduced treatment effectiveness
- Lower survival
There's no "stable" phase where the disease politely waits for you to be ready to diagnose it.
By the time you "feel worse enough" to get the scan, you may have missed your treatment window.
Would you wait to treat cancer until it spreads? Would you ignore diabetes until you go blind? Then why are you considering "waiting" on a progressive, fatal heart disease?
How to Actually Get the Scan (Action Plan)
Here's exactly what you need to do:
Step 1: Document Your Symptoms (TODAY)
Write down:
- All cardiac symptoms (shortness of breath, fatigue, swelling, etc.)
- All non-cardiac symptoms (carpal tunnel, neuropathy, GI issues, etc.)
- When symptoms started
- How they've progressed
- What makes them better or worse
- Family history of heart disease or amyloidosis
Step 2: Gather Your Medical Records
- Recent echo report
- ECG reports
- Blood test results (NT-proBNP, troponin if done)
- Any cardiac MRI or CT reports
- List of current medications
Step 3: See a Cardiologist (Preferably One Experienced in Amyloidosis)
Major medical centers in India with amyloidosis expertise include:
- AIIMS Delhi
- CMC Vellore
- Narayana Health, Bangalore
- Apollo Hospitals (major centers)
- Fortis Escorts, Delhi
- PGIMER Chandigarh
Step 4: Present Your Case Clearly
"Doctor, I've been reading about cardiac amyloidosis, and I'm concerned I might have it because I have [list your specific red flags]. I'd like to discuss whether a cardiac amyloid scan would be appropriate for me."
Step 5: If Met with Resistance
- Ask specific questions about why they don't think it's amyloidosis
- Request the clinical reasons for not ordering the scan
- Consider getting a second opinion
- Remember: You have the right to request specific tests, especially if you're paying for them
Step 6: Get the Scan
- Nuclear medicine departments in major hospitals
- Requires appointment scheduling
- Takes 2 imaging sessions the same day (initial and delayed imaging)
- Results typically in 1-2 days
Step 7: Follow Up with Results
- If positive: You need a comprehensive amyloidosis workup to determine type and extent in additipon to ruling out AL amyloidosis with appropriate blood tests.
- If negative: Work with cardiologist to find the correct diagnosis for your symptoms
The Financial Reality
Let's talk money because I know it matters:
Diagnostic Costs:
- Cardiac amyloid scan: ₹15,000 - 30,000
- Additional blood tests (to determine type): ₹5,000 - 15,000
- Genetic testing (if hereditary suspected): ₹25,000 - 50,000
- Total diagnostic workup: ₹45,000 - 95,000
Treatment Costs (Annual):
For ATTR with tafamidis:
- Medication: ₹10,00,000, - 12,00,000 per year
- Regular monitoring: ₹50,000 - 1,00,000 per year
- Total: ₹12,50,000 - 13,00,000 per year
For AL amyloidosis:
- Chemotherapy regimens: ₹3,00,000 - 10,00,000 (depending on protocol)
- Stem cell transplant: ₹10,00,000 - 20,00,000
- Supportive care: ₹1,00,000 - 3,00,000 per year
Yes, it's expensive. But consider:
Cost of Undiagnosed/Misdiagnosed Cardiac Amyloidosis:
- Years of wrong medications: ₹50,000 - 1,00,000 per year (wasted)
- Multiple hospitalizations: ₹1,00,000 - 3,00,000 per event (3-5 times per year)
- Advanced heart failure management: ₹5,00,000 - 15,00,000 annually
- End-stage care: ₹10,00,000 - 25,00,000+
- Lost years of life and productivity: INCALCULABLE
Plus, for tafamidis:
- Patient assistance programs exist
- Some insurance plans cover it
- Generic versions may become available
- Cost-benefit of extended life is undeniable
Your Heart's Final Plea
If your heart could speak to you right now, here's what it would say:
"For years, I've been trying to tell you something is different. I'm not just 'getting old.'
These protein deposits are suffocating me. They're making me stiff. I can't relax anymore between beats. I'm exhausted from trying to pump blood through my rigid walls.
Your symptoms aren't 'just heart failure.' They're my desperate cries for help.
That carpal tunnel you ignored? That was me, sending you a signal.
Those thickened walls on your echo? That was me, showing you something's wrong.
That fatigue you can't shake? That's me, failing slowly.
But here's the thing - there's a scan that can see what's happening to me. There are treatments that can help me survive longer, perform better.
Please. Don't wait until I can't send you signals anymore.
Don't wait until those protein deposits have strangled me completely.
Don't wait until the treatment options no longer work.
Get the scan. Find out what's really wrong. Give me - give US - a fighting chance.
Because once I stop completely, there's no restart button. And I'm not ready to leave you yet.
We have grandchildren to meet. Weddings to attend. Life to live.
But I need your help. I need that scan.
Please."
The Choice That Will Haunt You (Or Save You)
Close your eyes and imagine two scenarios:
Scenario 1:
Five years from now, you're sitting with your grandchild on your lap, reading a story. You're tired, yes, but stable. Your cardiac amyloidosis diagnosis from 5 years ago was scary, but you caught it in time. Treatment has given you these extra years. Years you almost missed.
You look at that little face looking up at you, and you think: "Thank God I got that scan."
Scenario 2:
Two years from now, your family is having a discussion with hospice. Your amyloidosis was diagnosed just 6 months ago - too late for the treatments to make much difference. The damage was already too extensive.
Your daughter is crying. Your grandchild, who you barely got to meet, will have no memories of you.
In your hospital bed, struggling to breathe, you have one recurring thought: "Why didn't I get that scan when I first read about it?"
Which scenario will be yours?
That decision starts today. Right now. In this moment.
What You Must Do RIGHT NOW
Not tomorrow. Not next week. Not "when I feel worse."
RIGHT. NOW.
Action Step 1: Check If You Need This Scan
Answer these questions honestly:
□ Do I have heart failure or heart failure symptoms? □ Am I over 60? □ Do I have unexplained thickened heart walls? □ Have I had carpal tunnel syndrome? □ Do I have numbness or tingling in my hands/feet? □ Does my heart failure not respond well to usual medications? □ Do I have a family history of early heart disease or amyloidosis?
If you checked 2+ boxes: You need to discuss an amyloid scan with a cardiologist.
Action Step 2: Book an Appointment
Don't think about it. Don't research more. Don't "wait and see."
Pick up your phone right now and call:
- Your current cardiologist
- A major teaching hospital's cardiology department
- A heart failure specialist at a tertiary care center
Book the earliest available appointment.
Action Step 3: Prepare for Your Appointment
- Print this article or save it on your phone
- Write down all your symptoms with dates
- Gather all your cardiac test reports
- Prepare your questions
- Bring a family member for support and to help remember details
Action Step 4: Be Your Own Advocate
- Don't accept vague reassurances
- Don't let anyone dismiss your concerns without explanation
- Ask directly about amyloidosis
- Request the scan if you meet criteria
- Get a second opinion if needed
Action Step 5: Follow Through
- Actually get the scan when ordered
- Show up for all imaging appointments
- Follow up for results
- If positive, pursue appropriate treatment
- If negative, continue seeking answers for your symptoms
The Accountability Moment
I'm going to ask you three questions. Answer them honestly:
Question 1: Do you have unexplained heart symptoms or any of the red flags mentioned in this article?
Question 2: Has your current cardiac diagnosis and treatment left you with lingering doubts or unresolved symptoms?
Question 3: If you died next year from undiagnosed cardiac amyloidosis, would your family wish you had read this article and taken action?
If you answered "yes" to any of these questions, you know what you need to do.
The Final Warning
Cardiac amyloidosis is the disease that hides in plain sight.
It mimics other conditions perfectly.
Standard tests miss it.
Most doctors don't think about it.
But that one scan - that single diagnostic test - can expose it.
Five years from now, you'll either be:
A) Grateful you took action today:
- Correctly diagnosed
- On appropriate treatment
- Alive to see your children grow
- Present for life's precious moments
- Living with a condition that's manageable
OR
B) One of the statistics:
- Diagnosed too late or not at all
- Missed treatment window
- Rapidly declining
- Full of regret
- Leaving your family too soon
The difference between these two futures is ONE SCAN.
One appointment.
One decision.
The scan costs ₹15,000 - 30,000.
Your life is worth infinitely more.
Take Action Now
If you suspect cardiac amyloidosis, need a second opinion, or want guidance on getting appropriate testing, don't delay—speak to a qualified cardiologist today.
Connect with experienced U.S.-based heart specialists for a comprehensive second opinion consultation to learn more about your health condition. They can review your case and guide you on whether cardiac amyloid imaging is appropriate for you:
👉 https://myamericandoctor.com/our-doctors/
You can also enroll in our soon-to-be-launched concierge medical clinic in India, Global Concierge Doctors. We provide comprehensive, US-style primary care with 24/7 access to India-based physicians to discuss any health concerns. Furthermore, we facilitate expert referrals to local Indian specialists and, if needed, US-based specialists to evaluate and manage your health conditions.
Your symptoms are real. Your concerns are valid.
The scan exists. The treatment exists.
Now the only question is: Will YOU take action?
Or will you close this tab and continue hoping those symptoms mean nothing?
Your heart is begging you to find out the truth.
Are you listening?
Reader Poll
Have you or a loved one been diagnosed with unexplained heart failure with preserved ejection fraction?
- Yes, and I never heard of amyloidosis
- Yes, and I've asked about amyloidosis but was told it's unlikely
- Yes, and I'm getting tested for amyloidosis now
- No, but this article has made me concerned
- I work in healthcare and this information is valuable
Share in the comments. Your story might save someone's life.
Share This Article
Know someone with:
- Unexplained heart failure?
- Thickened heart walls that don't make sense?
- Heart symptoms plus carpal tunnel?
- Heart failure that doesn't respond to usual treatment?
Share this article with them immediately.
That one share could add YEARS to their life.
Use the share buttons below or send them the direct link.
Sometimes a wake-up call from an outside source hits harder than family concern.
You might literally save a life by clicking "share."
Disclaimer
This article is for educational and awareness purposes only. It is not a substitute for professional medical advice, diagnosis, or treatment. Cardiac amyloidosis is a complex condition requiring expert evaluation. If you suspect you might have this condition, consult a qualified cardiologist or amyloidosis specialist immediately. Every person's medical situation is unique and requires personalized professional care.
Do you even know if your heart failure is really heart failure?
Or is it something else - something that has a name, a scan, and a treatment?
That scan is waiting for you.
The question is: Will you be in time?
Written with the urgent hope of catching this disease before it's too late. Share it forward. You might save a life.
Related Articles You Should Read:
- Understanding Heart Failure with Preserved Ejection Fraction (HFpEF)
- When Carpal Tunnel Syndrome Signals Heart Disease
- Advanced Cardiac Imaging: Beyond the Echo
- Gene Therapy and Amyloidosis: The Future of Treatment
Medical Disclaimer
This article is provided strictly for educational, informational, and awareness purposes only. It is not intended to be, and should not be construed as, professional medical advice, diagnosis, treatment, or a substitute for consultation with qualified healthcare professionals.
No Doctor-Patient Relationship
The information presented in this article does not establish a doctor-patient relationship between the reader and the author, publisher, or any affiliated entities. No medical decisions should be made based solely on the content of this article.
Consult Qualified Medical Professionals
If you are experiencing cardiac symptoms, chest pain, shortness of breath, unexplained fatigue, or any other health concerns mentioned in this article, seek immediate consultation with qualified cardiologists, physicians, or appropriate medical specialists. For medical emergencies, contact emergency services immediately.
Individual Medical Situations Vary
Every person's medical condition, health history, risk factors, and circumstances are unique. Diagnostic tests, treatment options, and medical recommendations must be tailored to individual patients through direct consultation with licensed healthcare providers who have access to complete medical histories and can perform proper clinical evaluations.
Not a Recommendation for Specific Tests or Treatments
References to Cardiac MRI, ECG, stress tests, echocardiograms, or any other diagnostic procedures in this article are for informational purposes only and do not constitute recommendations that you should or should not undergo these tests. All decisions regarding medical testing, diagnosis, and treatment should be made in consultation with qualified healthcare professionals based on your specific medical situation.
No Guarantee of Accuracy or Completeness
While efforts have been made to provide accurate information, medical knowledge continuously evolves. The information in this article may not reflect the most current research, clinical guidelines, or medical practices. The author and publisher make no representations or warranties regarding the accuracy, completeness, or timeliness of the content.
Do Not Disregard or Delay Professional Medical Advice
Never disregard, avoid, or delay obtaining professional medical advice from qualified healthcare providers because of something you have read in this article. If you have questions or concerns about information presented here, discuss them with your personal physician or cardiologist.
Third-Party Resources and Links
Any references to third-party medical services, clinics, doctors, or external websites are provided for informational purposes only and do not constitute endorsements. The author and publisher are not responsible for the content, services, or practices of any third-party entities.
Limitation of Liability
To the fullest extent permitted by law, the author, publisher, and affiliated entities disclaim all liability for any direct, indirect, incidental, consequential, or punitive damages arising from the use of, or reliance on, information contained in this article. This includes, but is not limited to, medical complications, financial losses, or any other adverse outcomes.
Geographic and Regulatory Considerations
Medical regulations, standards of care, insurance coverage, and availability of diagnostic tests vary by country, region, and healthcare system. Information regarding costs, procedures, and medical practices may not be applicable to all geographic locations or healthcare settings.
Your Responsibility
You acknowledge that you are solely responsible for your own health decisions and that you will consult with appropriate licensed healthcare professionals before making any medical decisions or undergoing any diagnostic tests or treatments.
Acknowledgment
By reading and using the information in this article, you acknowledge that you have read, understood, and agreed to this disclaimer in its entirety.
Last Updated: 30th January 2026
What's Your Reaction?
 Like
0
Like
0
 Dislike
0
Dislike
0
 Love
0
Love
0
 Funny
0
Funny
0
 Angry
0
Angry
0
 Sad
0
Sad
0
 Wow
0
Wow
0