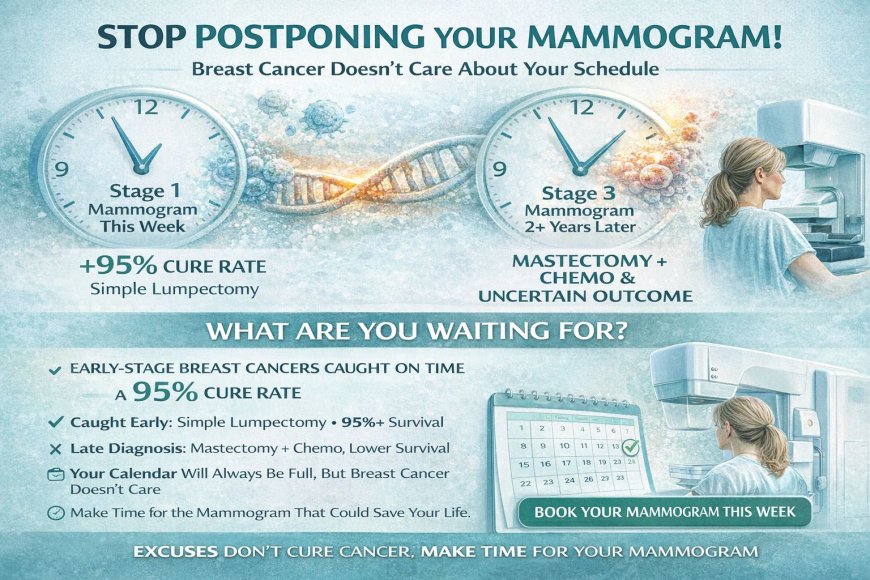
Breast Cancer Screening: The Mammogram You're 'Too Busy' to Schedule (And Why That Delay Could Kill You)
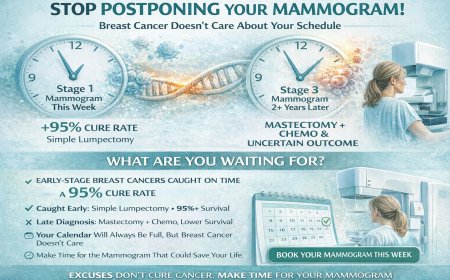
Postponing your mammogram isn't about being busy—it's about fear disguised as time management. While you reschedule for "next month," breast cancer doesn't wait. Early-stage cancers caught on mammograms at Stage 1 have over 95% cure rates with minimal treatment. The same cancers found two years later at Stage 3 require mastectomy, chemotherapy, and carry uncertain outcomes. That 20-minute mammogram you're avoiding could be the difference between a simple lumpectomy and months of devastating treatment. Stop making excuses. Book your screening this week. Your calendar will always be full, but breast cancer doesn't care about your schedule.
At A Glance
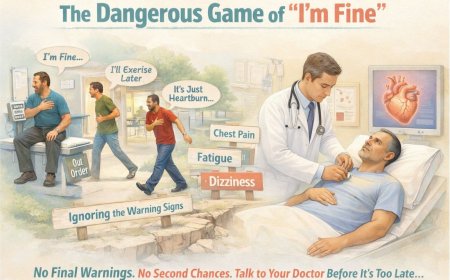
You're 42. Your doctor mentioned a mammogram two years ago. You nodded, fully intending to schedule it. Life got busy. Work deadlines. Kids' exams. Your mother's surgery. That home renovation. Always something more urgent than a test for a disease you don't have.
Except here's what you don't know: Right now, as you read this, approximately 1 in 28 to 1 in 29 Indian women will develop breast cancer in her lifetime. And the difference between catching it at Stage 1 versus Stage 3 often comes down to one thing — that mammogram you keep postponing.
This article reveals why your brain convinces you that you're "too busy" for 20 minutes that could save your life, what's silently growing in breast tissue while you reschedule, and why the appointment you make in the next 48 hours could be the most important decision of your entire life.
The Appointment You've Rescheduled Four Times
January 2024.
Your gynecologist hands you a prescription slip. "Time for your baseline mammogram. You're 40 now."
You fold it carefully, tuck it in your purse. "Definitely. I'll schedule it next month after this project deadline."
March 2024.
You find the crumpled slip while looking for your car keys. "Oh right, the mammogram. I'll do it after Diwali. Too much happening right now."
July 2024.
Annual checkup. Different doctor. Same conversation. New prescription. "I promise I'll do it this time. Just let me get through my daughter's wedding prep."
January 2025.
Another year. Another prescription. Another promise.
Meanwhile, in the tissue of your left breast, something microscopic that wasn't there 18 months ago has been quietly dividing. Doubling. Growing. Completely painless. Completely invisible to your touch. Completely catchable on a mammogram.
But you're too busy.
Sound familiar?
Here's The Brutal Truth About "Too Busy"
Let me tell you what "too busy" really means:
You're not too busy for a mammogram. You're too scared.
Scared of:
What they might find. The discomfort you've heard about. Taking time off work. Seeming paranoid or overly worried. Being "that woman" who makes her health a priority. Finding out you're not invincible.
So your brain, trying to protect you from fear, creates the perfect excuse: "I'm too busy."
It's not even a lie. You ARE busy. But here's the uncomfortable reality:
You're never going to NOT be busy.
There will always be a work deadline, a family function, a child's exam, a parent's need, a financial concern, a "better time."
The perfect moment to get a mammogram doesn't exist.
And while you're waiting for life to calm down, breast cancer doesn't wait. It doesn't care about your project deadline. It doesn't pause for weddings. It doesn't take a break during festival season.
It just grows.
What's Happening Inside Your Breast While You Reschedule
Let me walk you through what could be happening in those "too busy" months:
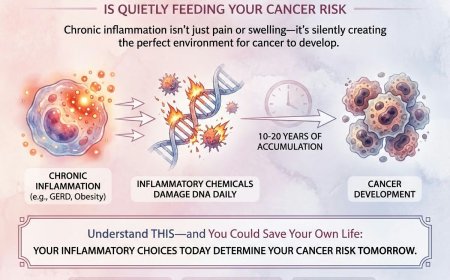
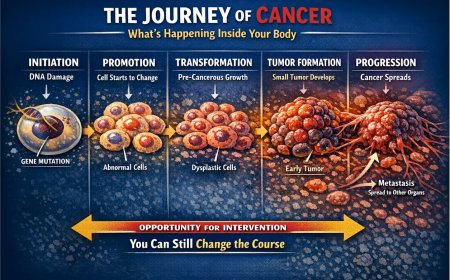
Months 1–6: The Silent Beginning
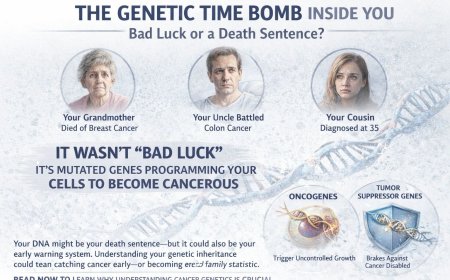
A single cell in your breast tissue mutates. Maybe from genetics. Maybe from environmental factors. Maybe just random bad luck.
That cell starts dividing abnormally. One becomes two. Two becomes four. Four becomes eight.
You feel nothing. No lump. No pain. No symptoms whatsoever.
A mammogram right now could detect it as a tiny cluster of calcifications. Treatment at this stage: possible lumpectomy, perhaps radiation. Survival rates at Stage 0 to Stage 1 are among the highest.
But you're rescheduling because of that work conference.
Months 6–12: The Critical Window
The abnormal cells continue multiplying. They may be forming a small mass — perhaps 5mm. Still too small for you to feel. Still invisible during your shower checks.
A mammogram could detect it now as a small, irregular mass. Treatment at this stage remains highly effective with strong long-term survival outcomes.
But you're postponing because of your daughter's board exams.
Months 12–18: The Point of Detection
The mass may now be approaching 1cm. You might be able to feel it only if you knew exactly where to look and how to examine yourself properly.
A mammogram would likely detect it clearly now. Treatment becomes more involved at this stage, potentially requiring more extensive surgery and adjuvant therapies. Survival rates, while still meaningful, begin to decline compared to earlier detection.
But you're delaying because of Diwali shopping.
Months 18–24: The Danger Zone
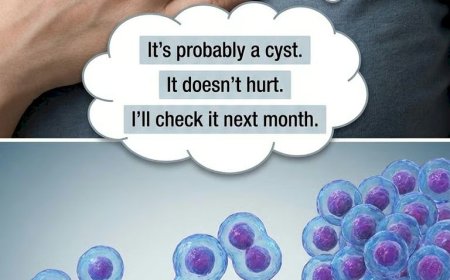
The tumor may now be 2cm. You may notice it in the shower and tell yourself it's "probably a cyst" or "just hormonal."
Cancer cells may have begun spreading to nearby lymph nodes. Treatment at this stage typically involves more aggressive interventions. Outcomes become significantly more uncertain.
But you're still "too busy."
Month 24+: The Regret
You finally see a doctor. Not because you scheduled that mammogram, but because the lump is now obvious. Or your breast shape has changed. Or there's a discharge from your nipple.
Diagnosis: Stage 3 breast cancer. It's in multiple lymph nodes.
Treatment: Mastectomy. Multiple rounds of chemotherapy. Radiation. Possible targeted therapy. Hair loss. Nausea. Fatigue. Uncertain future.
Your words: "If I'd just scheduled that mammogram when I was 40..."
Why Your Brain Is Literally Protecting You to Death
Let me explain the psychology behind your "too busy" excuse:
The Optimism Bias
Your brain is hardwired to believe bad things happen to OTHER people. Not you.
Breast cancer? That's something you read about. Something that happens to celebrities. Something in awareness campaigns. Not something that will actually affect YOUR body.
This bias makes you believe you have more time than you do.
The Discomfort Avoidance
You've heard mammograms are uncomfortable. Painful even. Your friend told you about the compression. Your sister complained about the cold room.
So your brain says: "Why subject yourself to discomfort when you probably don't even need it?"
Meanwhile, the temporary discomfort of a mammogram: 20 minutes.
The persistent discomfort of late-stage breast cancer treatment: months or years.
The "Young and Healthy" Delusion
"I'm only 42. Breast cancer happens to older women. I eat healthy. I exercise. I don't smoke. I'll get screened when I'm 50."
Reality: Breast cancer incidence in India is rising in younger women. Women in their 30s and 40s are increasingly being diagnosed. Indian women also tend to develop breast cancer at a younger age compared to Western counterparts. Waiting until 50 may mean waiting too long.
The Financial Concern
Let's put this simply: the cost of a mammogram is a fraction of the cost of treating advanced breast cancer. Early detection is, without question, the more financially sound decision — and far more importantly, the life-saving one. Check your health insurance policy. Many plans cover preventive screening including mammograms. Government hospitals and schemes in India often provide free or subsidised mammograms. If you need to plan for it, set aside a small monthly amount and protect your future.
Real Stories That Should Shake You Awake
Story #1: Meera, 44, Mumbai
Marketing executive. Always busy. Got her first mammogram recommendation at 40.
"I'll do it after this campaign launches." Then: "After my son's wedding." Then: "After we close the house deal."
Finally scheduled at 46 only because her company made it mandatory for health insurance renewal.
Mammogram result: Suspicious mass, right breast. Biopsy: Invasive ductal carcinoma, Stage 2B. Three lymph nodes positive.
Treatment: Mastectomy, six months of chemotherapy, radiation.
Her words: "I had four different prescriptions for mammograms over six years. FOUR. I kept all of them in my drawer like some kind of collection. If I'd gone at 40, they might have caught it at Stage 0 or 1. I might have kept my breast. I might have avoided chemo. But I was too busy. Too busy to spend 20 minutes that could have changed everything."
Story #2: Anjali, 39, Delhi
Ignored mammogram recommendations because "I'm not 40 yet, that's when screening starts."
Found a lump herself at 39 during Karva Chauth preparations.
By the time she got it checked: Stage 3A.
Her oncologist noted that an earlier baseline mammogram could have detected the cancer at a much earlier stage.
Treatment: Bilateral mastectomy, multiple rounds of dose-dense chemotherapy, radiation, ongoing hormone therapy.
She's alive. But she lost both breasts, her fertility, and two years of her life to treatment.
All because she waited for the "right age" to get screened.
Story #3: Divya, 51, Bangalore
Actually got regular mammograms from age 40 to 48. Then stopped. "I've been getting them for eight years. Everything's always fine."
Skipped for four years.
At 52, finally went back for screening after her friend was diagnosed.
Mammogram showed a mass with multiple suspicious lymph nodes.
Her radiologist noted it had likely been growing for two to three years — entirely missed because she stopped screening.
If she'd continued annual screening, it would likely have been caught much earlier.
Instead: Stage 3B. Extensive treatment. Uncertain prognosis.
The Seven Deadly Excuses (And Why They're Killing You)
Excuse #1: "I'm too young for breast cancer"
The Reality: Breast cancer rates are rising in younger Indian women. Women in their 30s and 40s are increasingly being diagnosed. Breast cancer doesn't check your age before forming.
Guidelines recommend baseline mammograms from age 40 (with the option from age 40–44 under ACS guidelines), but high-risk women should consult their doctor about starting earlier. If you have family history, genetic risk factors, or other concerns, don't wait to speak to a specialist.
Excuse #2: "Mammograms are painful"
The Reality: Uncomfortable? Yes, for about 20 minutes. Painful for most women? Closer to firm pressure than genuine pain. Unbearable? Absolutely not.
You know what's actually painful? Chemotherapy-induced neuropathy. Surgical drains after mastectomy. Radiation burns.
20 minutes of discomfort versus months of intensive treatment. Choose wisely.
Excuse #3: "There's no breast cancer in my family"
The Reality: Only 5–10% of breast cancers are linked to inherited genetic mutations like BRCA1 or BRCA2. That means 90–95% of breast cancer patients have no significant family history.
"No family history" does not equal "no risk."
Every woman with breast tissue carries some degree of risk. That's precisely why screening exists.
Excuse #4: "I do regular self-exams, so I'm covered"
The Reality: Breast self-awareness is encouraged — being familiar with how your breasts normally look and feel, and reporting any changes to your doctor promptly, remains valuable. However, it is important to note that the American Cancer Society does not currently recommend routine breast self-examination as a formal screening method for average-risk women, as research has not shown a clear benefit in reducing mortality when mammography is available.
What self-awareness cannot do is replace mammography. Mammograms can detect cancers as small as 2–3mm — far smaller than what the hand can feel. By the time you feel a lump, cancer may have been growing for months or years.
Self-awareness and mammography complement each other. One is not a substitute for the other.
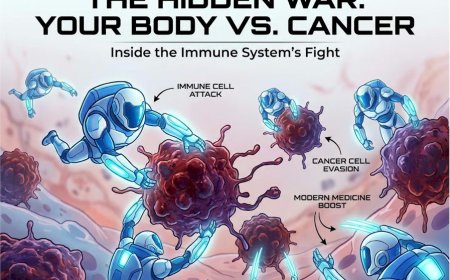
Excuse #5: "Mammograms aren't always accurate, so why bother?"
The Reality: No medical test is 100% accurate. Mammograms have a sensitivity of approximately 80–85% for standard 2D imaging, with improved rates for 3D tomosynthesis.
But you know what's less accurate? Not getting screened at all. That's 0% detection.
Modern mammography, especially 3D tomosynthesis, is more accurate than ever. Combined with ultrasound for dense breasts, detection rates improve significantly.
An imperfect test that saves lives is infinitely better than no test at all.
Excuse #6: "I can't afford it"
The Reality: Many Indian health insurance plans cover preventive screening including mammograms. Check your policy.
Government hospitals and schemes often provide free or subsidised mammograms for women who qualify.
And consider this: the cost of a mammogram, set aside through small monthly savings, is achievable for most. Your life is worth that planning effort.
Excuse #7: "I'll do it next year when I'm less busy"
The Reality: Next year, you'll be just as busy. There will always be something else. Always another excuse.
The calendar doesn't align with cancer growth. While you're waiting for a convenient time, cells are dividing.
There is no convenient time to have cancer. But there IS a convenient time to detect it early: NOW.
What Actually Happens During a Mammogram (It's Not What You Think)
Before the Test:
You'll be asked to avoid deodorant, powder, or lotion on your breasts or underarms. These can appear as white spots on X-rays. No fasting. No special preparation beyond that.
The Procedure:
You undress from the waist up and are given a gown. A technician — usually female — positions your breast on a flat plate. A second plate comes down to compress your breast. This compression spreads the tissue for a clearer image and also reduces radiation exposure. Each compression lasts around 10–15 seconds. The sensation is firm pressure, not unbearable pain. Two images per breast — top-to-bottom and side-to-side.
Total time: 15–20 minutes.
After the Test:
You can immediately return to all normal activities. No recovery time. No restrictions.
Results: Typically within 3–7 days.
That's it. 20 minutes. No needles. No anesthesia. No pain medication needed.
What About Dense Breasts?
If you have dense breast tissue — which is common in younger women and in Indian women — mammography may be supplemented with ultrasound. Your radiologist will recommend this if needed. Dense breasts do not necessarily mean higher cancer risk, but they do make imaging more challenging, which is why supplemental tools are sometimes used.
What You MUST Do in the Next 48 Hours
TODAY — Within the Next 2 Hours:
Check your age and risk factors. If you are 40 or older, you need a baseline mammogram now. If you are between 30–39 with family history or genetic risk factors, speak to your doctor about early screening.
Call and schedule. Don't spend hours comparing facilities. Pick one reputable radiology centre in your city and call today.
Major cities have excellent facilities. In Delhi: Sir Ganga Ram Hospital, Fortis, Max Healthcare. In Mumbai: Tata Memorial, Breach Candy, Lilavati. In Bangalore: Manipal Hospital, Apollo. In Chennai: Apollo, Fortis, MIOT.
Say: "I need to schedule a mammogram. What's your earliest appointment?" Book it. Even if it's three weeks away. Book it now.
Check your insurance. Call your health insurance provider and ask whether screening mammography is covered. Many policies cover preventive screening without co-pay.
Tell someone. Your spouse, mother, sister, or best friend. Say: "I've scheduled a mammogram for [date]. Please make sure I don't cancel."
Accountability matters.
TOMORROW:
Set reminders in your phone and email. Ask your accountability person to remind you.
Prepare your questions. When you go in, ask: "Do I have dense breasts? Do I need additional imaging?" and "Based on my results, when should I return?"
APPOINTMENT DAY:
Show up. Don't cancel. Don't reschedule.
Move the meeting. Skip the function if you must.
Your life is more important than any of these things.
Get your results. Ask when results will be available and follow up if you don't receive them. Don't assume "no news is good news." Get your actual results.
AFTER YOUR MAMMOGRAM:
Schedule your next one. If everything is normal, ask: "When should I come back?" Annual screening is the standard recommendation for most women aged 45–54. Put next year's appointment in your calendar today.
Share this article. Know other women who are "too busy" for mammograms? Share it. It might save a life.
Professional Support Options
If you're experiencing possible cancer symptoms, seeking a second opinion, or unsure which tests or treatments are right for you, don't wait. Speak with a qualified oncologist today.
Connect with experienced U.S.-based cancer specialists for a comprehensive second-opinion consultation. They will carefully review your case and help determine the most appropriate next steps for your individual health needs:
👉 https://myamericandoctor.com/our-doctors/
You may also choose to enroll in our upcoming concierge medical clinic in India, Global Concierge Doctors. We offer U.S.-style primary care with 24/7 access to India-based physicians for ongoing guidance on any health concern. When required, we coordinate referrals to trusted specialists in India and the U.S. for advanced evaluation and care.
Your health decisions today shape your life tomorrow.
The Final Word: Your Life Vs. Your Calendar
If that unscheduled mammogram could speak, here's what it would say:
"I'm 20 minutes. Twenty minutes that could tell you if there's something growing in your breast that you can't feel yet.
I'm 20 minutes that could catch cancer at Stage 1 instead of Stage 3.
I'm 20 minutes that could mean lumpectomy instead of mastectomy. Brief treatment instead of months of chemotherapy. Cure instead of uncertainty.
I'm 20 minutes you've been avoiding for two years because you're 'too busy.'
But here's the thing: If I find something today, you'll wish you'd come two years ago. Because two years of growth matters. Two years of spread matters. Two years could be the difference between life and death.
You check your phone 150 times a day. You spend time scrolling. You watch television in the evenings.
But you're too busy for 20 minutes that could save your life?
Your calendar will always be full. There will always be something else. Always another excuse.
But breast cancer doesn't care about your calendar. It doesn't wait for convenient times. It doesn't pause while you're busy.
It just grows.
So here's your choice: 20 minutes now for a mammogram. Or months later for treatment — if you're lucky enough to get that chance.
Stop being too busy to be alive."
Take Action NOW
Step 1: Stop reading right here.
Step 2: Pick up your phone.
Step 3: Call a radiology centre RIGHT NOW and book your mammogram.
Step 4: Tell someone you love that you've booked it.
Step 5: SHOW UP to your appointment. Don't cancel. Don't reschedule.
Your life is literally in your hands.
Reader Poll
Are you due for a mammogram?
[ ] Yes, and I'm scheduling it this week
[ ] Yes, but I've been postponing it
[ ] No, I get regular mammograms
[ ] Not yet at screening age but will when recommended
Medical Disclaimer
This article is provided strictly for educational, informational, and awareness purposes only. It is not intended to be, and should not be construed as, professional medical advice, diagnosis, treatment, or a substitute for consultation with qualified healthcare professionals.
No Doctor-Patient Relationship
The information presented in this article does not establish a doctor-patient relationship between the reader and the author, publisher, or any affiliated entities. No medical decisions should be made based solely on the content of this article.
Consult Qualified Medical Professionals
If you are experiencing any symptoms mentioned in this article, have been diagnosed with cancer, or have concerns about cancer risk, seek immediate consultation with qualified oncologists, physicians, or appropriate medical specialists. For medical emergencies, contact emergency services immediately.
Individual Medical Situations Vary
Every person's medical condition, health history, risk factors, cancer type, and circumstances are unique. Diagnostic tests, treatment options, and medical recommendations must be tailored to individual patients through direct consultation with licensed healthcare providers who have access to complete medical histories and can perform proper clinical evaluations.
Not a Recommendation for Specific Tests or Treatments
References to mammograms, biopsies, imaging studies (ultrasound, MRI), blood tests, chemotherapy, radiation therapy, immunotherapy, targeted therapy, surgery, or any other diagnostic procedures and treatments in this article are for informational purposes only and do not constitute recommendations that you should or should not undergo these tests or treatments. All decisions regarding medical testing, diagnosis, and treatment should be made in consultation with qualified healthcare professionals based on your specific medical situation.
No Guarantee of Accuracy or Completeness
While efforts have been made to provide accurate information, medical knowledge continuously evolves, particularly in the rapidly advancing field of oncology. The information in this article may not reflect the most current research, clinical guidelines, treatment protocols, or medical practices. The author and publisher make no representations or warranties regarding the accuracy, completeness, or timeliness of the content.
Do Not Disregard or Delay Professional Medical Advice
Never disregard, avoid, or delay obtaining professional medical advice from qualified healthcare providers because of something you have read in this article. If you have questions or concerns about information presented here, discuss them with your personal physician or oncologist.
Third-Party Resources and Links
Any references to third-party medical services, clinics, doctors, cancer centres, or external websites are provided for informational purposes only and do not constitute endorsements. The author and publisher are not responsible for the content, services, or practices of any third-party entities.
Limitation of Liability
To the fullest extent permitted by law, the author, publisher, and affiliated entities disclaim all liability for any direct, indirect, incidental, consequential, or punitive damages arising from the use of, or reliance on, information contained in this article. This includes, but is not limited to, medical complications, treatment decisions, or any other adverse outcomes.
Geographic and Regulatory Considerations
Medical regulations, standards of care, insurance coverage, availability of diagnostic tests, treatment protocols, and access to cancer therapies vary by country, region, and healthcare system. Information regarding procedures and medical practices may not be applicable to all geographic locations or healthcare settings.
Clinical Trials and Experimental Treatments
Any references to clinical trials, experimental treatments, or investigational therapies are for informational purposes only. Participation in clinical trials should only be considered after thorough discussion with your oncology team and understanding of all risks and benefits.
Your Responsibility
You acknowledge that you are solely responsible for your own health decisions and that you will consult with appropriate licensed healthcare professionals before making any medical decisions or undergoing any diagnostic tests or treatments.
Acknowledgment
By reading and using the information in this article, you acknowledge that you have read, understood, and agreed to this disclaimer in its entirety. You further acknowledge that this article has been created with the assistance of artificial intelligence. While every effort has been made to ensure accuracy, AI-generated content may occasionally contain errors, omissions, or inaccuracies. The information presented here is intended solely for educational and informational purposes and should not be relied upon as a substitute for professional medical advice. Readers are strongly encouraged to consult qualified healthcare professionals, refer to peer-reviewed medical literature, and cross-reference information from established clinical sources before making any health-related decisions.
Last Updated: 5th February 2026
What's Your Reaction?
 Like
0
Like
0
 Dislike
0
Dislike
0
 Love
0
Love
0
 Funny
0
Funny
0
 Angry
0
Angry
0
 Sad
0
Sad
0
 Wow
0
Wow
0