Aging and Cancer Risk: What You Can Control as Your Body Changes Over Time
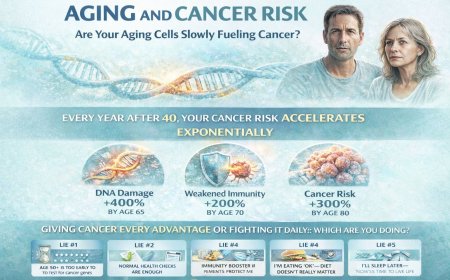
You're over 50. You feel fine. But inside, your cells are aging differently—DNA repair is slowing, your immune system is weakening, and cancer's odds are improving while yours decline. Every year after 40, cancer risk doesn't just increase—it accelerates exponentially. But here's what doctors won't tell you: while you can't stop aging, you CAN control whether you're giving cancer every advantage or fighting it daily. This article reveals the brutal biology of aging and cancer, the five deadly lies keeping you vulnerable, and the specific actions you must take in the next seven days to shift from aging into cancer to aging away from it.

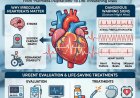
At A Glance
You're celebrating your 50th birthday. You feel fine. Healthy. Active. But inside your body, cells are dividing differently than they did at 30. Your DNA repair mechanisms are slowing. Your immune surveillance is weakening. And with each passing year, cancer's odds improve while yours get worse. This article reveals the brutal biology of aging and cancer, what you can't change, what you CAN control, and why the lifestyle choices you make TODAY could determine whether you're diagnosing cancer at 65 or celebrating your 85th birthday cancer-free.
The Birthday That Changes Everything (And You Don't Even Know It)
Age 50.
You blow out the candles. Take stock of your life. You're in decent shape. No major health issues. Maybe some creaky joints. Reading glasses. A few gray hairs.
You feel... fine.
Meanwhile, inside your body, something fundamental has shifted.
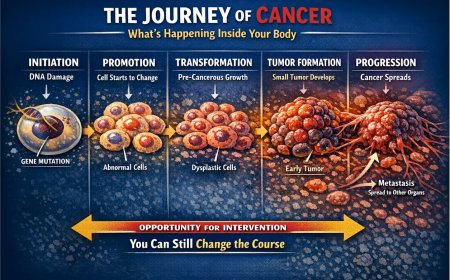
Your cells have divided hundreds of trillions of times since you were born. Each division carries a tiny risk of copying errors in your DNA. At 20, your body caught and fixed most of those errors. At 50? Your cellular repair crew is tired. Slower. Less efficient.
Think of it like a photocopier making copies of copies for 50 years. The first thousand copies? Perfect. The millionth copy? Errors start appearing. Lines. Smudges. Missing information.
That's your DNA at 50.
And cancer loves photocopier errors.
Here's what you're not being told: every year after 40, your cancer risk doesn't just increase — it accelerates. It's not linear. It's exponential.
At age 30, your lifetime cancer risk is relatively low. At age 50, that risk has multiplied several times. At age 70, it's multiplied again — and again.
But here's the part that should wake you up: while you can't reverse aging, you CAN control whether you're giving cancer every advantage or fighting it at every turn.
And most people over 50? They're unknowingly rolling out the red carpet for cancer cells.
The Brutal Biology: Why Cancer Loves Older Bodies
Let's be clear about what's happening inside your aging body that makes cancer more likely.
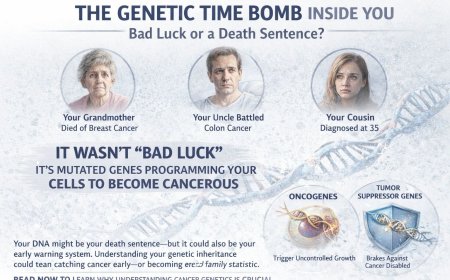
Cellular Mutation Accumulation (The Copycat Errors)
Every time a cell divides, there's a chance of DNA copying errors. Most get fixed. Some don't.
At age 20, cell division is fast and accurate, DNA repair is highly efficient, and accumulated mutations are minimal. At age 50, cell division becomes slower and more error-prone, DNA repair declines in efficiency, and accumulated mutations reach a significant burden. By age 70, error rates are climbing, DNA repair is markedly weakened, and the mutation burden becomes substantial.
Think of it as a game of genetic Russian roulette. At 20, you're playing with one bullet in a thousand chambers. At 70, you're playing with dozens of bullets in those same chambers. The longer you live, the more "bullets" accumulate.
But here's what you're missing: some of those bullets? You loaded them yourself.
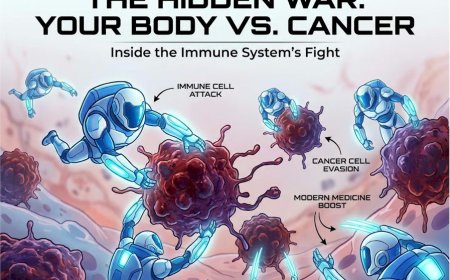
Immune System Decline (Your Body's Security Guards Getting Old)
Your immune system is supposed to identify and destroy abnormal cells, including early cancer cells. It's your body's 24/7 security team.
In your 20s and 30s, that security team is sharp, vigilant, and catches nearly every suspicious cell. In your 40s and 50s, the team is experienced but slower — some suspicious cells begin to slip through. By your 60s and beyond, the team is tired, understaffed, and missing more threats.
This phenomenon is called immunosenescence — the progressive aging of your immune system. Your T-cells, which hunt down abnormal cells, become less effective with each passing decade. Your natural killer cells, which destroy cancer cells, lose their killing power.
It's like having a security system that worked perfectly for 40 years, but now the cameras are fuzzy, the alarms are sluggish, and the guards fall asleep on duty.
And cancer cells notice.
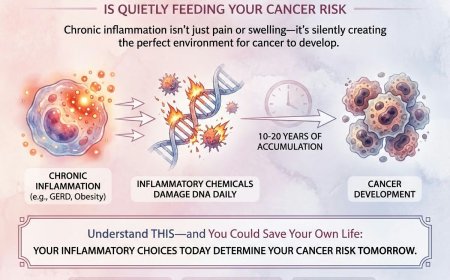
Chronic Inflammation (The Fire That Never Goes Out)
When you're young, inflammation is acute: you get injured, inflammation helps healing, then inflammation subsides. When you're older, inflammation becomes chronic — a low-grade fire burning constantly throughout your body.
This is called "inflammaging" — chronic, systemic inflammation that accompanies the aging process.
Why does it matter? Chronic inflammation creates an environment where cancer cells can thrive. It's like creating a warm, nutrient-rich environment for cancer to grow in.
What drives chronic inflammation as you age: accumulated cellular damage, persistent low-grade infections, visceral fat (belly fat), oxidative stress, and senescent cells — so-called zombie cells that won't die but no longer function normally.
You can't see it. You can't feel it. But it's there, day after day, year after year, quietly creating conditions that cancer can exploit.
The Five Deadly Lies About Aging and Cancer
Lie #1: "Cancer is just bad luck when you get older — nothing I can do about it"
The Brutal Reality: While age is a non-modifiable risk factor, lifestyle is MASSIVELY modifiable. Studies consistently show that lifestyle factors account for a substantial proportion of cancer cases. Your genes load the gun, but your lifestyle pulls the trigger.
What you CAN control: what you eat daily, how much you move, whether you smoke or drink, how you manage stress, whether you get screened regularly, your body composition, and your sleep quality. You're not powerless. You're choosing your cancer risk every single day through seemingly small decisions.
Lie #2: "I've smoked for 40 years — quitting now won't make a difference"
The Brutal Reality: This is perhaps the deadliest lie older adults tell themselves. Here's what happens when you quit smoking at any age: within weeks, lung function begins improving; within months, cancer-promoting inflammation starts decreasing; within years, cancer risk begins declining.
Yes, you've done damage. But continuing to smoke is like saying "I've already shot myself in the foot, might as well shoot the other one too." Every cigarette you DON'T smoke from this moment forward reduces your cancer risk. Period.
Lie #3: "I'm too old to change my diet or start exercising now"
The Brutal Reality: Your body responds to positive changes at ANY age. When you start exercising at 60, immune function improves, inflammation markers decrease, cellular repair mechanisms strengthen, and cancer risk factors decline. When you improve your diet at 65, antioxidant levels increase, DNA repair improves, hormone levels stabilize, and cancer-promoting inflammation decreases.
It's never too late to stop feeding cancer and start fighting it.
Lie #4: "My parents lived to 90 without cancer — I have good genes"
The Brutal Reality: Your parents didn't live in your world. They didn't eat ultra-processed foods filled with chemicals, sit for 12 hours a day, face modern pollution levels, experience chronic sleep deprivation, live in constant digital stress, or consume alcohol at the levels many people do today. Your genetic inheritance is not a shield — it's a head start you can easily squander through the choices you make in your environment.
Lie #5: "Getting screened more just finds things that wouldn't have mattered anyway"
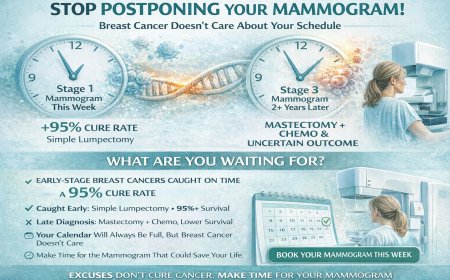
The Brutal Reality: This is the overdiagnosis argument, and while it has some merit in specific contexts, it's being used by many people as an excuse to avoid ALL screening. Early-stage cancers are vastly more treatable than late-stage cancers. Finding cancer at Stage 1 versus Stage 3 can mean the difference between a simple procedure and grueling treatment with uncertain outcomes. Yes, some cancers grow slowly. But you don't know which ones until they're found and properly evaluated. Would you rather find out you have a slow-growing cancer you can monitor — or find out you have an aggressive cancer that's already spread because you avoided screening?
Real Stories: The Choices That Determined Everything
Story #1: Ramesh, 58, Mumbai
The Situation: Ramesh smoked for 35 years. Two packs daily. His father died of lung cancer at 62.
The Turning Point: His daughter got married. He wanted to see grandchildren. He quit smoking at 56.
Two Years Later: A persistent cough. A chest X-ray showed a shadow. A CT scan confirmed early-stage lung cancer.
His doctor's words: "If you were still smoking, this would likely be Stage 3 or 4 by now. Because you quit two years ago, your lung tissue healed enough that we caught this early. You likely have years ahead of you."
Treatment: Surgical removal of the tumor. Clean margins. No chemotherapy needed.
Ramesh's reflection: "I thought quitting at 56 was pointless after 35 years of smoking. That decision may have saved my life. Every day I didn't smoke after quitting was a day my body healed a little more."
Story #2: Sunita, 62, Delhi
The Situation: Never exercised. Vegetarian diet but heavy on fried foods, sweets, and white rice. BMI of 32. Type 2 diabetes.
The Wake-Up Call: Her sister, age 65, was diagnosed with colorectal cancer. Sunita panicked and finally agreed to a colonoscopy she had been avoiding.
The Finding: Multiple polyps. Pre-cancerous. Removed during the colonoscopy itself.
Her doctor's recommendation: "Change your diet and lose weight. These polyps will come back if you don't address the root causes. Next time we might not catch them before they become cancer."
Her Action: Joined a walking group. Switched to whole grains. Cut out most fried foods and refined sugar.
18 Months Later: Lost 15 kg. Blood sugar normalized. Follow-up colonoscopy showed no new polyps.
Sunita's words: "At 62, I thought I was too old to change. I'm 64 now and in better shape than I was at 50. My sister's cancer saved my life because it scared me into action."
What You Can Control: Your Daily Cancer-Fighting Protocol
Here's the truth: you're aging. You can't stop that. But you CAN control whether you're aging into cancer or aging away from it.
1. Movement: Your Non-Negotiable Cancer Defense
The Science: Regular physical activity reduces cancer risk through multiple mechanisms — improving immune function, reducing inflammation, normalizing hormone levels, and improving insulin sensitivity.
What you're telling yourself: "I'm too old for exercise. My knees hurt. I'm too tired. I'll start next month."
The reality: every day you don't move is a day cancer has easier conditions to develop.
Your protocol: the minimum requirement is 150 minutes of moderate activity per week — that's 30 minutes, five days a week. Walking counts. Gardening counts. Swimming counts. Optimally, aim for 300 minutes of moderate activity per week, add strength training two to three days per week, and include flexibility work.
Start TODAY if you haven't: walk for 10 minutes after dinner tonight. Tomorrow: 12 minutes. The day after: 15 minutes. Build from there. You don't need a gym. You don't need equipment. You need commitment.
2. Food: Stop Feeding Cancer, Start Fighting It
The Science: Certain foods promote inflammation and cancer growth. Others fight both.
What you should limit or avoid: ultra-processed foods filled with preservatives, excessive red and processed meats, refined sugars and white flour, and trans fats.
What you should be eating more of: cruciferous vegetables (broccoli, cauliflower, cabbage), berries, dark leafy greens, whole grains, fatty fish rich in omega-3s, nuts and seeds, anti-inflammatory spices like turmeric and ginger, and green tea.
Your daily cancer-fighting plate should have half the plate as vegetables in a variety of colors, a quarter as whole grains or legumes, a quarter as lean protein, and a small amount of healthy fats.
Indian Context Specific Changes: Switch white rice to brown rice gradually (mix 50/50 to start). Replace maida-based foods with whole wheat or millets. Limit fried foods to once per week at most. Reduce cooking oil by 30–50%. Replace sugar-heavy sweets with fruit-based options. Use spices liberally — turmeric, ginger, and garlic are natural anti-inflammatories.
3. Body Composition: The Weight You Can't Ignore
The Science: Excess body fat, particularly visceral fat (belly fat), creates chronic inflammation and produces hormones that can promote cancer growth. Obesity is associated with an increased risk of multiple cancer types.
What you're telling yourself: "I've been this weight for 20 years. It's just how my body is. Losing weight at my age is impossible."
The reality: your "comfortable" weight may be creating cancer-friendly conditions inside your body.
Your action plan: if you're overweight, aim to lose 5–10% of your current body weight initially. This modest loss significantly reduces cancer risk factors. Combine mindful eating with increased movement. Focus on sustainable changes, not crash diets. Reduce portion sizes gradually, eliminate liquid calories such as sodas and sweetened drinks, eat slowly and mindfully, and track honestly what you eat for one week — you may be surprised.
4. Toxins: Stop Poisoning Yourself
Tobacco: if you smoke, quit. Today. Not next week. TODAY. Every cigarette increases cancer risk. Every cigarette NOT smoked reduces it.
Resources for quitting include nicotine replacement therapy, prescription medications (varenicline and bupropion), counseling and support groups, and mobile apps for tracking and motivation.
Alcohol: if you drink, limit it strictly. General guidance suggests no more than one standard drink per day for women and no more than two for men — but it is important to understand that no level of alcohol consumption is considered risk-free from a cancer prevention standpoint. Have alcohol-free days every week and never exceed safe limits.
Environmental Toxins: avoid tobacco smoke exposure including secondhand smoke, limit exposure to air pollution when possible, use natural cleaning products when feasible, and avoid unnecessary exposure to pesticides and chemicals.
5. Screening: Finding Cancer When It's Beatable
The Science: many cancers are highly treatable when caught early. The difference between Stage 1 and Stage 3 can be life or death.
Your age-appropriate screening schedule (discuss exact timing with your doctor based on your personal risk):
Colorectal Cancer (Ages 45–50+): colonoscopy every 10 years, or other approved screening tests more frequently. Earlier and more frequent screening if you have a family history of colorectal cancer.
Breast Cancer (Women): mammogram annually starting at age 45 for average-risk women (age 40–44 is an option to discuss with your doctor). Women 55 and older may choose to continue annually or transition to every two years. Continue as long as overall health is good and life expectancy is at least 10 years. The American Cancer Society no longer recommends routine breast self-exams or clinical breast exams as formal screening tools for average-risk women — mammography remains the gold standard. However, women should remain aware of how their breasts normally look and feel and report any changes to their doctor promptly.
Cervical Cancer (Women): Pap smear plus HPV test every five years, or Pap smear alone every three years, typically continuing until age 65 if prior screens have been normal.
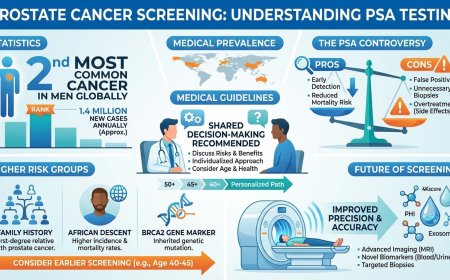
Prostate Cancer (Men): discuss PSA testing with your doctor starting at age 50. Earlier discussion at 45 is recommended if you are of African descent or have a family history of prostate cancer. Understand both the potential benefits and the limitations of this test.
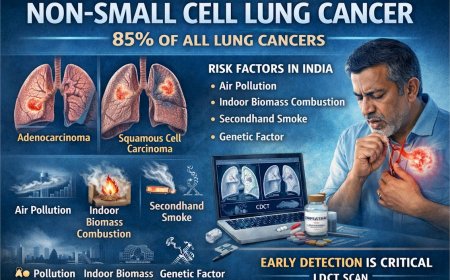
Lung Cancer: annual low-dose CT scan if you are between the ages of 50 and 80 AND have a significant smoking history. Discuss with your doctor whether you qualify.
Skin Cancer: annual full-body skin evaluation by a dermatologist is advisable. Be alert to any new or changing moles or skin lesions and seek evaluation promptly.
What you're telling yourself: "Screenings are invasive. Uncomfortable. If something's wrong, I don't want to know."
The reality: finding cancer at Stage 1 is ALWAYS easier and more survivable than finding it at Stage 3 or 4. The temporary discomfort of a colonoscopy is nothing compared to the permanent consequences of undetected colorectal cancer.
6. Sleep: The Repair Time Your Cells Desperately Need
The Science: during deep sleep, your body repairs DNA damage, strengthens immune function, and removes cellular waste. Chronic sleep deprivation impairs all of these cancer-fighting mechanisms.
Your protocol: aim for 7–8 hours nightly, maintain a consistent sleep schedule with the same bedtime and wake time, sleep in a dark and cool room, avoid screens for at least one hour before bed, and address sleep apnea if suspected — symptoms include loud snoring and daytime fatigue.
Poor sleep isn't just making you tired. It's weakening your defenses against cancer.
7. Stress Management: Turning Off Chronic Fight-or-Flight
The Science: chronic stress weakens immune function, promotes inflammation, and may accelerate cellular aging.
Your protocol: develop a daily stress-reduction practice such as meditation, prayer, or deep breathing. Maintain regular social connection — social isolation is associated with poorer health outcomes including increased cancer risk. Address chronic anxiety or depression with professional help. Find purpose and meaning in daily life.
What You MUST Do in the Next 7 Days
Stop reading. Start acting.
Day 1 (TODAY): schedule any overdue cancer screenings, throw out cigarettes if you smoke, and take a 15-minute walk after dinner. Day 2: track everything you eat for one full day honestly, check your BMI (weight in kg divided by height in meters squared), and walk for 20 minutes. Day 3: make one meal swap (white rice to brown rice, or fried to baked), identify your single biggest cancer risk factor, and walk for 25 minutes. Day 4: make a specific plan to address your biggest risk factor, tell someone you trust about this plan, and walk for 30 minutes. Day 5: research smoking cessation programs if applicable, buy vegetables you don't normally eat, and walk for 30 minutes. Day 6: cook one cancer-fighting meal heavy on vegetables and whole grains, set a consistent bedtime for the next 30 days, and walk for 30 minutes. Day 7: review the week — what worked, what was hard — adjust your plan for the following week, walk for 30 minutes, and commit to the next seven days.
Professional Support Options
If you're experiencing possible cancer symptoms, seeking a second opinion, or unsure which tests or treatments are right for you, don't wait. Speak with a qualified oncologist today.
Connect with experienced U.S.-based cancer specialists for a comprehensive second-opinion consultation. They will carefully review your case and help determine the most appropriate next steps for your individual health needs:
👉 https://myamericandoctor.com/our-doctors/
You may also choose to enroll in our upcoming concierge medical clinic in India, Global Concierge Doctors. We offer U.S.-style primary care with 24/7 access to India-based physicians for ongoing guidance on any health concern. When required, we coordinate referrals to trusted specialists in India and the U.S. for advanced evaluation and care.
Your health decisions today shape your life tomorrow.
The Final Word: Your Aging Body's Message to You
If your cells could speak, here's what they'd say:
"I've divided trillions of times to keep you alive. I'm getting tired. Making mistakes. My repair crew is slowing down. But I'm still fighting. Every healthy meal you eat gives me ammunition. Every walk you take strengthens my defenses. Every cigarette you don't smoke reduces my burden. Every screening catches problems I couldn't fix on my own. I can't stop aging. But together, we can stop giving cancer easy victories. Your choices in the next decade will determine if I become cancer-ridden or cancer-resistant. Help me fight. I'm still fighting for you."
Take Action NOW
Step 1: Schedule any overdue cancer screenings — colonoscopy, mammogram, PSA, lung CT — whatever applies to you. Step 2: Identify your single biggest modifiable cancer risk factor. Step 3: Make ONE change today addressing that risk. Step 4: Tell someone who will hold you accountable. Step 5: Set a calendar reminder for 30 days to assess your progress.
You're aging. That's inevitable. Whether you're aging INTO cancer or AWAY from it? That's your choice. Make it today.
Reader Poll
What's your biggest barrier to cancer prevention?
☐ I don't think I'm at risk ☐ I'm too busy to make lifestyle changes ☐ I'm scared of what screenings might find ☐ I don't know where to start ☐ I've already scheduled my screenings and started changes
Share This Article
Know someone over 50 who's ignoring their cancer risk? Know someone who thinks "I'm too old to change now"? Share this article. It might add years to their life.
Medical Disclaimer
This article is provided strictly for educational, informational, and awareness purposes only. It is not intended to be, and should not be construed as, professional medical advice, diagnosis, treatment, or a substitute for consultation with qualified healthcare professionals.
No Doctor-Patient Relationship
The information presented in this article does not establish a doctor-patient relationship between the reader and the author, publisher, or any affiliated entities. No medical decisions should be made based solely on the content of this article.
Consult Qualified Medical Professionals
If you are experiencing any symptoms mentioned in this article, have been diagnosed with cancer, or have concerns about cancer risk, seek immediate consultation with qualified oncologists, physicians, or appropriate medical specialists. For medical emergencies, contact emergency services immediately.
Individual Medical Situations Vary
Every person's medical condition, health history, risk factors, cancer type, and circumstances are unique. Diagnostic tests, treatment options, and medical recommendations must be tailored to individual patients through direct consultation with licensed healthcare providers who have access to complete medical histories and can perform proper clinical evaluations.
Not a Recommendation for Specific Tests or Treatments
References to biopsies, imaging studies (CT scans, PET scans, MRI), blood tests, tumor markers, chemotherapy, radiation therapy, immunotherapy, targeted therapy, surgery, or any other diagnostic procedures and treatments in this article are for informational purposes only and do not constitute recommendations that you should or should not undergo these tests or treatments. All decisions regarding medical testing, diagnosis, and treatment should be made in consultation with qualified healthcare professionals based on your specific medical situation.
No Guarantee of Accuracy or Completeness
While efforts have been made to provide accurate information, medical knowledge continuously evolves, particularly in the rapidly advancing field of oncology. The information in this article may not reflect the most current research, clinical guidelines, treatment protocols, or medical practices. The author and publisher make no representations or warranties regarding the accuracy, completeness, or timeliness of the content.
Do Not Disregard or Delay Professional Medical Advice
Never disregard, avoid, or delay obtaining professional medical advice from qualified healthcare providers because of something you have read in this article. If you have questions or concerns about information presented here, discuss them with your personal physician or oncologist. Early detection and prompt treatment significantly improve cancer outcomes.
Third-Party Resources and Links
Any references to third-party medical services, clinics, doctors, cancer centers, or external websites are provided for informational purposes only and do not constitute endorsements. The author and publisher are not responsible for the content, services, or practices of any third-party entities.
Limitation of Liability
To the fullest extent permitted by law, the author, publisher, and affiliated entities disclaim all liability for any direct, indirect, incidental, consequential, or punitive damages arising from the use of, or reliance on, information contained in this article. This includes, but is not limited to, medical complications, treatment decisions, or any other adverse outcomes.
Geographic and Regulatory Considerations
Medical regulations, standards of care, availability of diagnostic tests, treatment protocols, and access to cancer therapies vary by country, region, and healthcare system. Information regarding procedures and medical practices may not be applicable to all geographic locations or healthcare settings.
Clinical Trials and Experimental Treatments
Any references to clinical trials, experimental treatments, or investigational therapies are for informational purposes only. Participation in clinical trials should only be considered after thorough discussion with your oncology team and understanding of all risks and benefits.
Your Responsibility
You acknowledge that you are solely responsible for your own health decisions and that you will consult with appropriate licensed healthcare professionals before making any medical decisions or undergoing any diagnostic tests or treatments.
Acknowledgment
By reading and using the information in this article, you acknowledge that you have read, understood, and agreed to this disclaimer in its entirety. You further acknowledge that this article has been created with the assistance of artificial intelligence. While every effort has been made to ensure accuracy, AI-generated content may occasionally contain errors, omissions, or inaccuracies. The information presented here is intended solely for educational and informational purposes and should not be relied upon as a substitute for professional medical advice. Readers are strongly encouraged to consult qualified healthcare professionals, refer to peer-reviewed medical literature, and cross-reference information from established clinical sources before making any health-related decisions.
Last Updated: 5th February 2026
What's Your Reaction?
 Like
0
Like
0
 Dislike
0
Dislike
0
 Love
0
Love
0
 Funny
0
Funny
0
 Angry
0
Angry
0
 Sad
0
Sad
0
 Wow
0
Wow
0