When Your Heart Gives Up and Nobody Knows Why: The Terrifying Reality of Unexplained Heart Failure
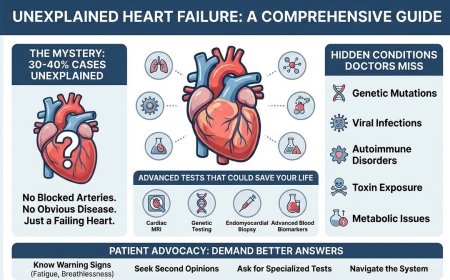
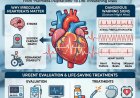
Unexplained heart failure strikes without warning—your heart suddenly can't pump blood effectively, but doctors can't find the cause. No blocked arteries. No obvious disease. Just a failing heart and mounting fear. This comprehensive guide reveals why 30-40% of heart failure cases remain unexplained, the hidden conditions doctors often miss, and the advanced tests that could save your life. Learn the warning signs, when to demand better answers, and how to navigate the medical system when standard tests show nothing but your symptoms tell a different story.
The Medical Mystery That's Killing Thousands
You're exhausted. Not just tired — bone-deep, can't-catch-your-breath exhausted.
Your ankles are swollen. You wake up gasping for air at 2 AM. Climbing one flight of stairs feels like running a marathon.
Your cardiologist runs tests. ECG. Echocardiogram. Blood work. Stress test. Coronary angiogram.
Everything comes back "relatively normal" or "no significant blockages."
Your doctor says: "Your heart function is reduced, but we can't find a clear cause. It's idiopathic heart failure."
Idiopathic. Medical speak for: "We don't know why your heart is failing."
And you're supposed to just... accept that?
The Medical Mystery That's Killing Thousands
Here's what nobody tells you about heart failure: a significant proportion of heart failure cases — estimates range widely depending on the population studied and the depth of the diagnostic workup — have no clearly identified cause at the time of initial diagnosis. That's not a small number. That's a large group of people walking around with failing hearts while being told "we're not sure why."
But here's the terrifying truth: "Unexplained" doesn't mean there's no cause. It means the cause hasn't been found yet.
And the difference between finding that cause and not finding it? It could be the difference between effective treatment and progressive disability leading to death.
What "Heart Failure" Actually Means (And Why It's Worse Than You Think)
Let's be clear about what we're talking about. Heart failure doesn't mean your heart has stopped. It means your heart can't pump enough blood to meet your body's needs.
Think of your heart as a pump that's supposed to deliver blood efficiently throughout your body with every contraction. In heart failure, that pump weakens. Circulation becomes inadequate, especially during exertion and physiological stress — and sometimes even at rest as the condition progresses.
What happens when your organs don't receive enough blood, or when fluid backs up because the heart cannot keep up?
Your brain suffers — confusion, difficulty concentrating, and memory problems can become routine. Your kidneys struggle, leading to fluid retention and swelling in the legs and abdomen. Your lungs can fill with fluid, causing shortness of breath, especially when lying flat. Your muscles waste, producing profound fatigue and the inability to exert yourself in any meaningful way. Your digestive system becomes congested, bringing nausea, loss of appetite, and abdominal bloating.
Every organ in your body can start faltering because your heart — the master pump — can no longer do its job. This is not a slow inconvenience. It is a systemic cascade of organ dysfunction that, if left unaddressed, can become irreversible.
The Story Nobody Wants to Hear (But You Need To)
Priya's Story
Priya was 48. Healthy all her life. Never smoked. No diabetes. Normal cholesterol. Active lifestyle.
She started feeling tired in March. By May, she couldn't walk to her mailbox without stopping to catch her breath. Her legs were so swollen she couldn't wear regular shoes.
Her local cardiologist ran all the standard tests. Nothing explained it.
"Must be stress," he said. "Maybe early menopause. Lose some weight."
She got sicker. By July, she was admitted to the hospital with acute heart failure. Her ejection fraction — a measure of how well the heart pumps — had dropped from a normal 55–60% to 25%. She was critically ill, and nobody knew why.
Finally, a specialist ordered advanced testing: cardiac MRI with late gadolinium enhancement and comprehensive genetic testing.
The diagnosis: a pregnancy-associated cardiomyopathy history that had never been fully investigated, combined with a genetic mutation associated with progressive heart muscle weakness. Nobody had looked for it because the assumption was that pregnancy-related cardiomyopathy would not still be relevant after many years.
She is now on appropriate treatment. Her heart function has improved significantly. She is alive.
But she nearly died because "unexplained" was accepted as a final answer.
The Ten Hidden Causes Doctors Often Miss
When heart failure is called "unexplained," it usually means one of the following conditions was not properly investigated.
1. Viral Myocarditis (Inflammation from Infection)
A viral infection — sometimes as common as influenza or COVID-19 — can inflame the heart muscle. The acute phase of the infection passes, but the damage can remain silently in the tissue.
Why it's missed: Standard blood tests performed weeks or months after the infection may show nothing abnormal. Cardiac MRI with late gadolinium enhancement can detect scarring and tissue patterns consistent with prior myocarditis. Viral myocarditis is responsible for a meaningful percentage of dilated cardiomyopathy presentations, especially in younger patients.
2. Genetic Cardiomyopathies
Some people inherit genetic mutations that cause the heart muscle to weaken, thicken, or develop abnormally. These conditions do not typically appear at birth — they often manifest in the 30s, 40s, or 50s, long after any obvious warning signs might have been expected.
Why it's missed: Doctors frequently do not order genetic testing unless there is an obvious family history. However, many cardiomyopathy-causing mutations can be de novo — meaning they arise spontaneously, with no prior family history at all.
Recognized genetic cardiomyopathies include dilated cardiomyopathy, where the heart chambers enlarge and weaken; hypertrophic cardiomyopathy, where the heart muscle thickens abnormally; arrhythmogenic right ventricular cardiomyopathy, a condition in which heart muscle is progressively replaced by fatty and fibrous tissue; and left ventricular non-compaction, where the heart muscle fails to develop the compact structure it needs to function efficiently.
3. Toxin-Induced Cardiomyopathy
Something you are being exposed to is damaging your heart muscle, often over years and without dramatic warning signs.
Common culprits include alcohol consumed consistently over years. Chemotherapy agents such as anthracyclines (doxorubicin) and trastuzumab (Herceptin) are well-documented cardiac toxins. Environmental exposures to heavy metals — lead, mercury, and arsenic among them — can silently damage heart muscle. Certain medications, including some antipsychotics and antiretroviral drugs, carry cardiac toxicity profiles. Recreational substances such as cocaine and methamphetamines can directly damage myocardial tissue.
Why it's missed: Physicians do not always take thorough occupational and exposure histories. Patients frequently underreport alcohol consumption or fail to mention herbal and supplemental remedies they do not consider "medications."
4. Nutritional Deficiencies
The heart muscle requires specific micronutrients to generate energy, maintain structure, and contract properly. When these are absent, the heart can weaken — and standard blood panels will never reveal it unless the right tests are ordered.
Thiamine (vitamin B1) deficiency can cause wet beriberi, a form of high-output heart failure, particularly relevant in individuals with heavy alcohol use or malabsorption conditions. Selenium deficiency is directly linked to Keshan disease, a dilated cardiomyopathy first identified in selenium-deficient regions of China. Carnitine is essential for transporting fatty acids into cardiac mitochondria for energy production; deficiency can result in metabolic cardiomyopathy. Coenzyme Q10 plays a central role in mitochondrial energy production in heart cells; statin medications reduce endogenous CoQ10 synthesis, and the clinical significance of this in heart failure patients remains an active area of research.
Why it's missed: Standard metabolic panels do not include these measurements. Nutritional deficiency is often dismissed unless the patient appears obviously malnourished.
5. Stress-Induced Cardiomyopathy (Takotsubo)
Severe emotional or physical stress can trigger a sudden, dramatic weakening of the heart muscle — a condition the Japanese call Takotsubo cardiomyopathy, sometimes referred to as "broken heart syndrome."
Triggers include the sudden death of a loved one, major physical trauma, serious surgery, sudden catastrophic news, or extreme emotional shock. The condition can mimic a heart attack in presentation, but the coronary arteries may be clear. In many cases, heart function recovers within weeks to months with appropriate management.
Why it's missed: Without awareness of the diagnosis, it is easily dismissed as anxiety or attributed to an acute coronary event, and the potentially reversible nature of the condition is never recognized.
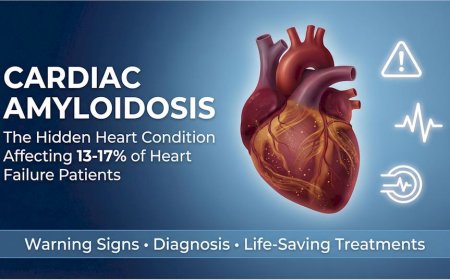
6. Infiltrative Diseases
In infiltrative cardiomyopathies, abnormal substances deposit within the heart muscle, making it progressively stiff, thickened, and unable to fill or pump properly.
Cardiac amyloidosis occurs when misfolded proteins accumulate in heart tissue. It has two primary forms: AL amyloidosis, associated with plasma cell disorders, and transthyretin amyloidosis (ATTR), which can be hereditary or age-related and is now recognized as significantly underdiagnosed, particularly in older adults. Sarcoidosis is an inflammatory condition in which granulomatous deposits infiltrate cardiac tissue, causing heart block, arrhythmias, and heart failure. Hemochromatosis involves toxic iron accumulation in the heart and other organs, often from a hereditary iron metabolism disorder. Fabry disease is a rare X-linked lysosomal storage disorder in which lipid accumulation damages the heart muscle over time.
Why they're missed: These are conditions outside the standard diagnostic framework for many general cardiology evaluations. They require specific blood tests, specialized cardiac MRI sequences, and in some cases nuclear imaging to identify.
7. Thyroid Dysfunction
Both an overactive thyroid (hyperthyroidism) and an underactive thyroid (hypothyroidism) can directly cause or significantly worsen heart failure. Hypothyroidism can reduce cardiac contractility and promote fluid retention. Hyperthyroidism can drive persistent high-output demand that, over time, strains the myocardium.
Why it's missed: The symptoms of thyroid dysfunction overlap substantially with those of heart failure itself, and thyroid function tests are not universally included in the initial workup.
8. Obstructive Sleep Apnea
Obstructive sleep apnea causes repeated episodes of oxygen deprivation during sleep. Each episode triggers surges in blood pressure and sympathetic nervous system activation. Over months and years, this places extreme mechanical and metabolic stress on the heart.
Sleep-disordered breathing is present in a substantial proportion of heart failure patients, and frequently goes unrecognized because neither the patient nor the physician connects disrupted sleep to cardiac decline.
Why it's missed: Physicians do not routinely order sleep studies as part of cardiac workup. The connection between sleep-disordered breathing and heart failure progression is underappreciated in general cardiology practice.
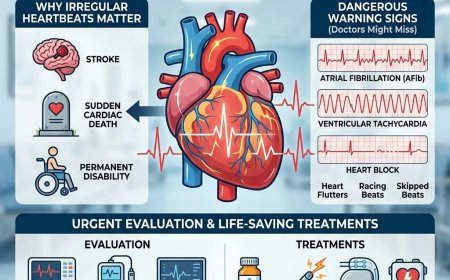
9. Tachycardia-Induced Cardiomyopathy
When the heart beats persistently and abnormally fast — most often due to uncontrolled atrial fibrillation or other sustained tachyarrhythmias — the myocardium eventually exhausts itself. This is not always a result of intrinsic heart muscle disease. It can be a direct consequence of relentless rate demand placed on the heart.
Crucially, tachycardia-induced cardiomyopathy is often substantially or completely reversible once the heart rate is controlled and the rhythm is appropriately managed. Failure to recognize it means treating the consequence while ignoring the cause.
Why it's missed: The rapid heart rate is acknowledged and managed, but the causal link to the cardiomyopathy is not established until rate control is achieved and heart function is reassessed.
10. Peripartum Cardiomyopathy
Peripartum cardiomyopathy is heart failure that develops in the final month of pregnancy or within five months of delivery. While it is commonly associated with the immediate postpartum period, pregnancy can also unmask underlying vulnerability, including genetic dilated cardiomyopathy, and delayed recognition can occur when symptoms were never fully investigated at the time.
Why it's missed: Physicians do not routinely take pregnancy histories spanning more than a few years, and women themselves often attribute persistent fatigue and exertional symptoms to aging or stress rather than a cardiac condition associated with pregnancy.
The Diagnostic Failure: Why "Unexplained" Is Actually "Uninvestigated"
Here is the honest reality about why so many cases of heart failure remain without a cause.
The standard cardiac workup typically includes an ECG, an echocardiogram, basic blood work, and sometimes a stress test or coronary angiogram. This workup answers a narrow set of questions: Are there significant coronary blockages? Is the heart pumping weakly? Are the valves functioning? Are there rhythm disturbances?
What this workup often cannot tell you is why the heart muscle is weak. It may not reliably detect inflammation within the tissue. It may not identify scarring from older viral infections. It may not find infiltrative deposits. It may not reveal genetic mutations. It may not assess nutritional adequacy at the cellular level. It may not detect toxin exposure. It may not evaluate sleep-related physiological stress.
It is the equivalent of investigating a complex crime scene by examining only the body, while declining to analyze fingerprints, interview witnesses, review security footage, or perform forensic analysis. You know something happened. You simply have no idea what.
Accepting an "unexplained" label after a standard workup is not a diagnosis. It is the absence of one.
The Advanced Tests Your Doctor Should Order (But Probably Won't Unless You Ask)
If your heart failure has no identified cause and you want actual answers, the following investigations represent the next tier of a thorough diagnostic evaluation.
Cardiac MRI with Late Gadolinium Enhancement
Cardiac MRI with late gadolinium enhancement is one of the most powerful tools for myocardial tissue characterization. It can identify patterns of scar tissue that suggest specific underlying diseases — myocarditis can leave characteristic non-ischemic scarring patterns; ischemic damage can produce subendocardial or transmural enhancement; amyloidosis can produce diffuse enhancement patterns; sarcoidosis can show patchy scarring. None of these patterns are visible on standard echocardiography. In appropriate patients with unexplained cardiomyopathy, cardiac MRI is a strongly evidence-supported next step.
Comprehensive Genetic Testing Panel
A genetic testing panel covering the major cardiomyopathy genes can identify inherited mutations even in patients with no apparent family history. The results carry implications not only for the patient but for biological relatives who may be silently carrying the same mutation. Pathogenic variants in genes such as LMNA, SCN5A, MYH7, MYBPC3, PKP2, and others have established clinical implications for risk assessment and management.
Cardiac PET Scan
Cardiac positron emission tomography with FDG (fluorodeoxyglucose) is particularly valuable for detecting active cardiac inflammation such as sarcoidosis, and PET-based protocols can also be used in certain settings to assess myocardial perfusion and viability.
Endomyocardial Biopsy
Endomyocardial biopsy — the sampling of small pieces of heart muscle tissue during cardiac catheterization — can provide tissue-level diagnosis when non-invasive tests are inconclusive. It remains a definitive diagnostic option for selected forms of myocarditis, infiltrative disease, and storage disorders. While it carries procedural risks and is not indicated in all cases, it can be essential when the clinical picture is compelling and the therapeutic decision hinges on a tissue diagnosis.
Comprehensive Nutritional Testing
Specific micronutrient testing — thiamine, selenium, carnitine, coenzyme Q10, vitamin D, magnesium, and complete iron studies including ferritin and transferrin saturation — can identify deficiencies that are correctable and that standard panels may not detect.
Sleep Study (Polysomnography)
A formal sleep study is a straightforward and non-invasive investigation that should be considered in patients with unexplained heart failure symptoms and risk factors for sleep apnea, given the high prevalence of sleep-disordered breathing in this population and evidence that treatment can improve outcomes in appropriate patients.
Complete Thyroid Function Panel
A full thyroid panel — including TSH, free T4, free T3, and thyroid antibodies — can help rule out thyroid-driven cardiac dysfunction and identify autoimmune thyroid disease.
Toxicology Screen and Heavy Metal Testing
In patients with relevant exposure histories, testing for alcohol biomarkers, heavy metals (lead, mercury, arsenic), and recreational or occupational chemical exposures can identify a reversible contributor and guide treatment.
The Questions That Will Change Your Doctor's Approach
When your doctor says "unexplained heart failure," you do not have to accept it. These specific questions reframe the conversation.
"Have you ordered a cardiac MRI with late gadolinium enhancement to look for specific patterns of scarring or inflammation that standard echocardiography cannot detect?"
Cardiac MRI can identify an underlying diagnosis in a meaningful proportion of patients whose echocardiogram does not clarify etiology. In appropriate cases, it is a medically justified next step in unexplained cardiomyopathy.
"Should we pursue genetic testing for cardiomyopathy, given that this condition has developed without a clear cause?"
Genetic testing can influence risk assessment, guide screening of relatives, and sometimes change management.
"Could this be related to a viral infection I experienced months or years ago?"
This question opens the door to a discussion about myocarditis — a diagnosis that can be overlooked when the acute infection has already passed.
"Have we systematically ruled out infiltrative diseases such as amyloidosis, sarcoidosis, or hemochromatosis?"
These conditions require tests outside the basic workup. Naming them directly compels a clear answer about whether they’ve been considered.
"Could any medication, supplement, substance, or environmental exposure be contributing to this?"
This prompts a thorough exposure history and can reveal modifiable causes.
"Should I have a sleep study to evaluate for obstructive sleep apnea?"
Given the prevalence of sleep-disordered breathing in heart failure, this can be an entirely reasonable request in the right clinical context.
"Have we assessed my nutritional status comprehensively, including thiamine, selenium, and carnitine?"
Nutritional cardiomyopathies can be missed if not specifically tested.
"Would an endomyocardial biopsy be appropriate in my case to obtain a definitive tissue diagnosis?"
This prompts a careful discussion of benefits, risks, and indications.
What "Unexplained" Really Costs You
Let's be very direct about what accepting "unexplained" as a final answer means for your future.
Without a specific diagnosis, treatment remains generic and may be suboptimal for the underlying cause. Standard heart failure medications — ACE inhibitors, beta-blockers, diuretics, mineralocorticoid antagonists — are valuable foundations, but they are not sufficient for every underlying etiology. Cardiac sarcoidosis may require immunosuppression. Toxin-induced cardiomyopathy requires removal of the offending agent. Nutritional deficiencies require targeted correction. Transthyretin amyloidosis now has approved disease-modifying therapy (tafamidis) that can alter the disease course. Treating the syndrome while ignoring the cause is medicine's equivalent of mopping up a flood while the pipe is still bursting.
Without a genetic diagnosis, your family may remain at risk. If a heritable mutation is driving your heart failure, your children and siblings may be carrying the same variant silently. Early identification and monitoring can reduce the risk of advanced disease developing unnoticed.
Without a clear cause, it can be difficult to determine whether your treatment is working optimally, or whether an ongoing pathological process is still causing damage beneath the surface.
And without answers, you carry an enormous psychological burden — the weight of not knowing why your body is failing you, whether you caused it, and whether it will inevitably destroy you.
With a specific diagnosis, the picture changes. Targeted treatment becomes possible. Family members can be identified and protected. Prognosis becomes clearer. Emerging therapies — including gene-based treatments now in development for inherited cardiomyopathies — may become relevant. And perhaps most importantly, you are no longer fighting an invisible enemy.
The Brutal Reality: How Long Do You Have?
Heart failure prognosis depends enormously on underlying cause — and this is precisely why the distinction between "unexplained" and "diagnosed" matters so profoundly.
In mild heart failure with ejection fractions in the 40–50% range, those with unidentified causes may face ongoing risk of progression without cause-specific intervention, while those with reversible causes — including alcohol-related cardiomyopathy, tachycardia-induced cardiomyopathy, or nutritional deficiency — may see substantial improvement once the underlying driver is addressed.
In moderate heart failure, long-term outcomes vary widely by etiology, severity, response to therapy, comorbid conditions, and access to appropriate follow-up. Reversible causes can carry substantially better trajectories when identified and treated. Advanced infiltrative disease and certain genetic cardiomyopathies can carry worse trajectories if not recognized and managed appropriately.
In severe heart failure with ejection fractions below 30%, outcomes without advanced therapies can be poor — but even here, etiology matters. Some causes remain partially reversible even at advanced stages. Advanced therapies including implantable devices, mechanical circulatory support, and cardiac transplantation can be life-extending when appropriate.
The difference between knowing your diagnosis and not knowing it is not academic. It can represent years of additional functional life.
When Your Doctor Won't Order Advanced Tests: The Second Opinion Strategy
It happens too often. You ask for cardiac MRI or genetic testing and your cardiologist responds: "It's unlikely to change management," or "The tests we've done are sufficient," or "Let's manage your symptoms and see how you do."
When the reason for heart failure remains unclear and symptoms are significant, it is reasonable to seek clarity on the decision-making.
Step 1: Request Written Documentation of the Clinical Reasoning
"Dr. [Name], I understand your position on further testing. Could you please document in my medical records the clinical rationale for why cardiac MRI and genetic testing are not indicated in my case? I'd like this documented for my records."
This is appropriate. It is your right as a patient to understand the reasoning behind clinical decisions.
Step 2: Seek a Second Opinion at a Specialized Center
Seeking a second opinion is standard practice for complex or unexplained conditions. You are entitled to one. If unexplained heart failure persists despite standard evaluation, consultation with a heart failure subspecialist or a cardiomyopathy program is a reasonable next step.
In India, institutions with advanced cardiac imaging capabilities and heart failure subspecialty programs include AIIMS New Delhi, PGIMER Chandigarh, Christian Medical College Vellore, and major tertiary centers such as Fortis Escorts Heart Institute, Apollo Hospitals, and Medanta.
When requesting a second opinion, a respectful and effective way to frame it is: "Dr. [Name], I genuinely appreciate the care you have provided. Because we have not yet identified the underlying cause of my heart failure and my symptoms continue to significantly affect my daily functioning, I would like a second opinion from a heart failure subspecialist. Would you be able to provide my complete records, imaging reports, and test results for their review?"
Good physicians will support this.
The Five Critical Warning Signs That Mean "Get Answers NOW"
If you have unexplained heart failure and any of the following are present, the urgency for advanced diagnostic workup escalates immediately.
Rapid Progression: Your ejection fraction is declining significantly over months. This can suggest an ongoing destructive process — not a stable condition to be observed.
Age Under 50: Heart failure at a young age without an obvious cause increases concern for genetic, inflammatory, or infiltrative disease. Identification has implications for biological relatives.
Family History: Early heart disease, unexplained sudden cardiac death, or known cardiomyopathy in close relatives increases the probability of a heritable condition.
Associated Systemic Symptoms: Peripheral neuropathy, unexplained kidney dysfunction, vision changes, significant unexplained weight loss, or skin manifestations alongside heart failure can suggest systemic disease — including amyloidosis, sarcoidosis, or Fabry disease — that requires specialized evaluation.
Treatment Non-Response: Standard heart failure therapy is not improving symptoms or cardiac function. This can suggest that cause-specific treatment may be needed, not only optimization of generic therapy.
The Action Plan: What to Do Starting Today
Stop accepting "unexplained" as a final answer.
This Week:
Document everything systematically — your complete symptom timeline, every illness and infection you have had in the past several years, your complete medication and supplement history, your alcohol history (honestly), any occupational or environmental exposures, your pregnancy history if applicable, and your family history of cardiac disease or sudden death.
Obtain copies of all your test results — not summaries, but actual reports with numbers and images.
Research which hospitals in your area have cardiac MRI capability and heart failure subspecialty programs.
Within Two Weeks:
Schedule a consultation with a heart failure specialist — not a general cardiologist unless they have a specific subspecialty focus in cardiomyopathy. Prepare a written list of questions. Bring a family member to take notes and provide additional history.
Request discussion of the following investigations when clinically appropriate: cardiac MRI with late gadolinium enhancement, a genetic cardiomyopathy panel, comprehensive nutritional testing, a sleep study referral, and a complete thyroid function panel including antibodies.
Within One Month:
Complete ordered investigations. If advanced testing is refused without adequate clinical justification, pursue a second opinion at a specialized center.
If a genetic cause is identified or strongly suspected, organize appropriate screening for first-degree relatives — your children, siblings, and parents may require evaluation.
Ongoing:
Track your response to treatment systematically. Document daily weight, symptom severity, and activity tolerance. Follow up with repeat echocardiography as advised by your clinician to track ejection fraction trends. Know your numbers.
The Uncomfortable Questions You Must Ask Yourself
Before you move on from this article, answer these honestly.
Are you willing to live the rest of your life not knowing why your heart is failing — accepting that there might be a reversible cause that is never discovered?
If this condition is genetic and your children develop the same disease because genetic testing was never pursued — could you live with that?
What are you actually afraid of — the investigation itself, or what the investigation might find?
If you were told definitively that a two-year delay in diagnosis would cost you twenty years of life — would you act differently today?
Are you accepting your doctor's diagnostic limitations as your own?
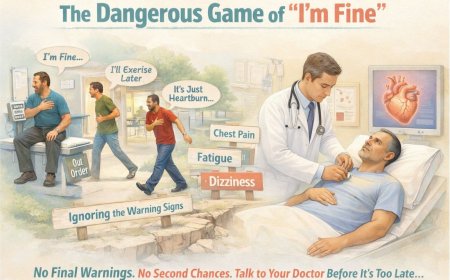
Why Your Heart Doesn't Care About Your Excuses
Your heart doesn't care that advanced testing takes time to arrange. It doesn't care that pursuing answers feels like more effort than you have. It doesn't care that you don't want to seem like a difficult patient or that you're trying to avoid confronting bad news.
Your heart only cares about one thing: whether it is receiving what it needs to survive.
Every day without a diagnosis is another day the underlying cause — whether inflammation, infiltration, toxin exposure, metabolic deficiency, or genetic vulnerability — may continue doing damage. Some of that damage can be reversible if caught in time. Some of it will become permanent.
The window for intervention does not stay open indefinitely.
The One Thing That Separates Survivors from Victims
I have seen two types of heart failure patients.
The first accepts "unexplained" as a final answer. They take their medications. Their symptoms gradually worsen. Their quality of life declines. Eventually they face advanced interventions they might have avoided, or they die prematurely from a condition that may have been treatable.
The second refuses to accept "unexplained" as a final answer. They pursue comprehensive diagnostic evaluation. They seek multiple opinions. They find answers. They receive targeted treatment. Many stabilize. Some improve substantially. Many live years or decades longer than their initial trajectory suggested.
The difference between these two patients is persistence and self-advocacy.
Your cardiologist sees dozens of patients every week. You have one life. Who has more reason to fight for the answer?
What Happens If You Do Nothing?
The trajectory of undiagnosed, generically managed heart failure follows a recognizable pattern.
In the first year or two, symptoms remain at a manageable if diminished level. Medications multiply. Appointments become more frequent. Life narrows imperceptibly but steadily.
By years three and four, the decline accelerates. Hospitalizations for fluid overload become part of the calendar. Work becomes difficult or impossible. Simple activities require rest afterward.
By years five and six, severe limitation defines daily existence. Dependence on others for basic tasks increases. Advanced therapies enter the conversation — implantable defibrillators, cardiac resynchronization devices, mechanical circulatory support.
Beyond that point, the choices narrow to heart transplantation for those who qualify, or end-of-life planning for those who don't.
Now contrast this against the alternative: an identified diagnosis, targeted treatment, a heart function that stabilizes or improves, and a life that continues — with work, with family, with travel, with purpose — a decade from now.
The actions you take in the next 30 days shape which of these futures becomes yours.
The Final Message: Your Heart's Last Request
If your failing heart could speak to you right now, this is what it would say:
"I have been with you since before you took your first breath. I have never stopped. Never complained. Never asked for anything in return. But I am struggling now. Something is wrong with me — something that may be diagnosable, something that might be treatable.
Please don't accept 'we don't know why' as the last word. Please fight for me the way I have been fighting for you every single day of your life.
Please get me to specialists who have the tools to see what is really wrong. Please give me a chance at proper treatment, not just a lifetime of managed decline.
I don't want to fail you. But I cannot keep fighting an unknown enemy while we pretend that not knowing why is acceptable.
Please. Demand answers. Pursue testing. Seek specialists.
Because once I give up completely, there is no coming back. And I don't want to leave you yet. We have so much more life to live together.
This may be my last request. Please listen."
Take Action NOW
You've read this far. That means you know, in your heart, that "unexplained" isn't good enough.
Hours 1–24:
Save this article and share it with your family. Write down your complete symptom and exposure history. List every question you have about your condition.
Hours 24–48:
Obtain copies of all your medical records and test results. Research heart failure centers and subspecialists in your area. Call and schedule an appointment with a heart failure specialist.
Hours 48–72:
Prepare for your specialist appointment with organized documentation. Make a list of the advanced tests you want to discuss. Identify family members who may need evaluation if a genetic cause is found.
Don't wait. Every day matters when your heart is failing.
Professional Support Options
If you're experiencing possible cancer symptoms, seeking a second opinion, or unsure which tests or treatments are right for you, don't wait. Speak with a qualified oncologist today.
Connect with experienced U.S.-based cancer specialists for a comprehensive second-opinion consultation. They will carefully review your case and help determine the most appropriate next steps for your individual health needs:
👉 https://myamericandoctor.com/our-doctors/
You may also choose to enroll in our upcoming concierge medical clinic in India, Global Concierge Doctors. We offer U.S.-style primary care with 24/7 access to India-based physicians for ongoing guidance on any health concern. When required, we coordinate referrals to trusted specialists in India and the U.S. for advanced evaluation and care.
Your health decisions today shape your life tomorrow.
Medical Disclaimer
This article is provided strictly for educational, informational, and awareness purposes only. It is not intended to be, and should not be construed as, professional medical advice, diagnosis, treatment, or a substitute for consultation with qualified healthcare professionals.
No Doctor-Patient Relationship
The information presented in this article does not establish a doctor-patient relationship between the reader and the author, publisher, or any affiliated entities. No medical decisions should be made based solely on the content of this article.
Consult Qualified Medical Professionals
If you are experiencing cardiac symptoms, chest pain, shortness of breath, unexplained fatigue, or any other health concerns mentioned in this article, seek immediate consultation with qualified cardiologists, physicians, or appropriate medical specialists. For medical emergencies, contact emergency services immediately.
Individual Medical Situations Vary
Every person's medical condition, health history, risk factors, and circumstances are unique. Diagnostic tests, treatment options, and medical recommendations must be tailored to individual patients through direct consultation with licensed healthcare providers who have access to complete medical histories and can perform proper clinical evaluations.
Not a Recommendation for Specific Tests or Treatments
References to Cardiac MRI, ECG, stress tests, echocardiograms, genetic testing, or any other diagnostic procedures in this article are for informational purposes only and do not constitute recommendations that you should or should not undergo these tests. All decisions regarding medical testing, diagnosis, and treatment should be made in consultation with qualified healthcare professionals based on your specific medical situation.
No Guarantee of Accuracy or Completeness
While efforts have been made to provide accurate information, medical knowledge continuously evolves. The information in this article may not reflect the most current research, clinical guidelines, or medical practices. The author and publisher make no representations or warranties regarding the accuracy, completeness, or timeliness of the content.
Do Not Disregard or Delay Professional Medical Advice
Never disregard, avoid, or delay obtaining professional medical advice from qualified healthcare providers because of something you have read in this article.
Third-Party Resources and Links
Any references to third-party medical services, clinics, doctors, or external websites are provided for informational purposes only and do not constitute endorsements.
Limitation of Liability
To the fullest extent permitted by law, the author, publisher, and affiliated entities disclaim all liability for any direct, indirect, incidental, consequential, or punitive damages arising from the use of, or reliance on, information contained in this article.
Geographic and Regulatory Considerations
Medical regulations, standards of care, insurance coverage, and availability of diagnostic tests vary by country, region, and healthcare system.
Your Responsibility
You acknowledge that you are solely responsible for your own health decisions and that you will consult with appropriate licensed healthcare professionals before making any medical decisions or undergoing any diagnostic tests or treatments.
Acknowledgment
By reading and using the information in this article, you acknowledge that you have read, understood, and agreed to this disclaimer in its entirety. You further acknowledge that this article has been created with the assistance of artificial intelligence. While every effort has been made to ensure accuracy, AI-generated content may occasionally contain errors, omissions, or inaccuracies. The information presented here is intended solely for educational and informational purposes and should not be relied upon as a substitute for professional medical advice. Readers are strongly encouraged to consult qualified healthcare professionals, refer to peer-reviewed medical literature, and cross-reference information from established clinical sources before making any health-related decisions.
For Medical Emergencies: Contact your local emergency services immediately or go to the nearest emergency room.
Have you or a loved one been told you have "unexplained heart failure"? What steps did you take to find answers? Share your story in the comments — your experience might help someone else navigate this challenging journey.
What's Your Reaction?
 Like
0
Like
0
 Dislike
0
Dislike
0
 Love
0
Love
0
 Funny
0
Funny
0
 Angry
0
Angry
0
 Sad
0
Sad
0
 Wow
0
Wow
0