The Nuclear Cardiology Second Opinion - When Your Heart Sends Mixed Signals - That Could Save Your Life
Received inconclusive, equivocal, or borderline stress test results? Before proceeding with invasive cardiac catheterization or dismissing concerning findings, understand why nuclear cardiology second opinions can be life-saving. This comprehensive guide reveals the dangerous "gray zone" where unclear test results lead to either unnecessary invasive procedures or missed heart disease diagnoses. Learn the five critical signs that demand expert review, understand what makes stress tests inconclusive, and discover how specialized nuclear cardiology interpretation prevents catastrophic mistakes. We explain the real costs of diagnostic uncertainty, debunk the myth that second opinions offend doctors, and provide actionable steps to access world-class cardiac imaging specialists through virtual consultations. Whether you're facing conflicting medical opinions or questioning your cardiologist's recommendations, this article empowers you with knowledge to make informed decisions about your cardiac health. Don't let unclear test results determine your fate—get expert clarity before it's too late.
Your stress test came back.
The doctor says it's "inconclusive." Or "equivocal." Maybe there are "some abnormalities, but we're not sure what they mean."
Your cardiologist mentions catheterization. Says it's "probably necessary."
You feel fine. Or maybe you don't. But those test results? They're telling two different stories.
Sound familiar?
Here's what nobody tells you: Inconclusive test results often lead to unnecessary, invasive cardiac procedures that carry the risk of life-threatening complications.
The Dangerous Space Between "Normal" and "Emergency"
You are currently at a critical stage in your diagnostic journey:
The Gray Zone.
Not sick enough for immediate intervention. Not healthy enough to ignore. Somewhere in that terrifying middle where decisions get made based on incomplete information.
And here's the uncomfortable reality:
Wrong decisions in this gray zone lead to unnecessary invasive procedures—or missed heart attacks.
Let me be brutally honest about what's at stake.
The Two Mistakes That My Occur
Mistake #1: The Unnecessary Catheterization
Your doctor sees an "abnormal" stress test. To be "safe," they recommend cardiac catheterization.
Sounds reasonable, right? Better safe than sorry?
Here's what actually happens:
3:00 AM: You're admitted to the hospital, fasting, anxious, unable to sleep.
7:00 AM: They wheel you into the cath lab. Thread a catheter through your groin artery, up through your body, into your heart. You're awake for all of it.
7:30 AM: The procedure reveals... nothing. Your arteries are perfectly fine. The stress test was a false alarm.
But now you've undergone an invasive procedure you didn't need. You have:
- A puncture wound in your groin that takes weeks to heal properly
- Exposure to radiation (equivalent to 200-500 chest X-rays)
- Risk of complications: bleeding, infection, artery damage, allergic reactions
- Medical bills: ₹50,000 - 1,00,000
- Lost work days: 3-7 days minimum
- Psychological trauma: anxiety about your heart condition
All because an inconclusive test was interpreted as "abnormal."
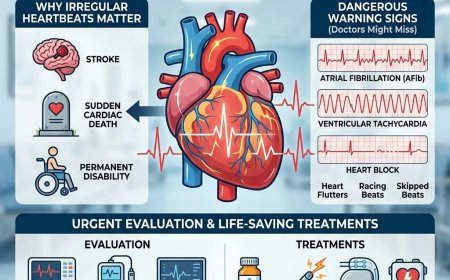
Mistake #2: The Missed Diagnosis
Or worse—far worse—the opposite happens.
Your stress test shows "some changes, but probably nothing serious." Your doctor says, "Let's just monitor it. Come back in six months."
You go home relieved. You feel fine. You continue your normal life.
Three months later: Massive heart attack while driving. You crash your car. You're lucky to survive.
When they finally do the catheterization you should have had three months ago, they find severe three-vessel coronary artery disease. Your arteries were 80-90% blocked.
The stress test actually DID show the disease. But the interpretation was wrong. The subtle findings were dismissed as "probably nothing."
Your heart tried to warn you. The test captured it. But the interpretation failed you.
The Brutal Truth About "Inconclusive" Results
Let me explain what "inconclusive" actually means in medical-speak:
It means: "I don't know. I'm not certain. This could mean something serious, or it could mean nothing. I'm guessing."
Your doctor won't say it that way. They'll use professional language: "equivocal findings," "non-diagnostic," "borderline," "possibly artifactual."
But the reality is: When test results are unclear, interpretation becomes educated guesswork.
And here's the terrifying part:
Two equally qualified cardiologists can look at the same inconclusive stress test and reach opposite conclusions.
One says: "Needs immediate catheterization."
Another says: "Probably fine, just monitor it."
Who's right? Your life depends on the answer.
The Story of Sharma Uncle: A Cautionary Tale
Vikram Sharma, 58, software executive in Bengaluru.
Monday: Stress test shows "non-specific ST-segment changes." His cardiologist is puzzled. Results don't clearly show heart disease, but they're not completely normal either.
Tuesday: The cardiologist decides to be "conservative." Prescribes medications, says come back in three months.
Wednesday: Vikram goes to work, relieved. Tells his wife the doctor said not to worry.
Thursday: Chest discomfort during an evening walk. He thinks it's indigestion. Takes an antacid.
Friday morning: Collapses at breakfast table. Cardiac arrest.
His wife performs CPR until the ambulance arrives. They save him—barely.
Friday afternoon: Emergency catheterization reveals severe left main coronary artery disease—the "widow-maker" blockage. He needs emergency bypass surgery.
He survives. But he shouldn't have been that close to death.
A nuclear cardiology expert reviewing his stress test later said:
"The findings were subtle but definitely abnormal. This patient needed immediate further evaluation. The test wasn't inconclusive—it was misinterpreted."
One expert opinion. One week earlier. Would have changed everything.
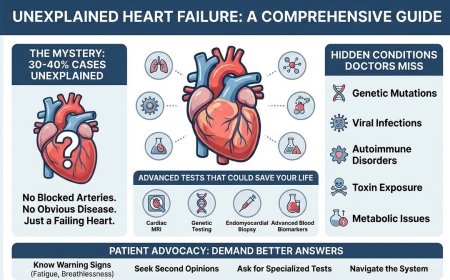
What Makes Stress Tests "Inconclusive"? The Technical Reality
Let me explain what's actually happening when results are unclear:
Common Causes of Inconclusive Results:
1. Patient-Related Factors:
- You couldn't exercise enough (due to joint pain, breathing problems, fatigue)
- Your baseline ECG has abnormalities (prior heart attack, bundle branch block)
- You're on medications that affect the test (beta-blockers, digoxin)
- You have left ventricular hypertrophy from high blood pressure
2. Technical Factors:
- Poor image quality on nuclear scans
- Artifacts that look like abnormalities but aren't (breast tissue, diaphragm movement)
- Borderline perfusion defects that could be disease—or just normal variation
- ECG changes that could be ischemia—or could be something else entirely
3. Test Limitations:
- Standard exercise only stress tests miss 30-40% and nuclear stress tests miss about 10-15% of significant coronary disease
- Women often have more false positives than men
- Obese patients have technical challenges with imaging
When test results are unclear, it takes specialized expertise to determine what's real disease and what's artifact or normal variation.
Your general cardiologist is good. But nuclear cardiology specialists do nothing but interpret these complex scans all day, every day. They see patterns others miss.
The Five Signs You Absolutely Need a Second Opinion
Stop and answer these questions honestly:
1. Are your test results described with any of these phrases?
- "Equivocal"
- "Non-diagnostic"
- "Borderline abnormal"
- "Possibly artifactual"
- "Cannot rule out ischemia"
- "Non-specific changes"
- "Difficult to interpret"
If YES: You need a nuclear cardiology expert to review the actual images, not just the report.
2. Are you being recommended for catheterization based solely on an unclear stress test?
Red Flag Alert: If your only symptom is an equivocal test result, and you're being sent for invasive procedures, you need another expert opinion first.
3. Do you have risk factors that make interpretation more complex?
- Previous heart attack
- Prior coronary stent or bypass surgery
- Left bundle branch block
- Pacemaker
- Severe obesity (BMI >35)
- Significant breast tissue (for women)
If YES: Standard interpretation may not apply to you. You need specialized expertise.
4. Did you have a pharmacological stress test instead of exercise?
Nuclear stress tests may be performed with exercise or with pharmacologic stress agents (medications like adenosine, regadenoson or dobutamine). If your results are unclear, expert review is crucial.
5. Are two doctors telling you completely different things?
If you've already gotten conflicting opinions, you need a nuclear cardiology specialist to be the tiebreaker—an expert who can definitively interpret those subtle findings.
What a Nuclear Cardiology Second Opinion Actually Involves
Let me demystify this process:
What Is Nuclear Cardiology?
It's a sub-specialty focused on cardiac imaging using radioactive tracers. These specialists:
- Interpret thousands of nuclear stress tests annually
- Recognize subtle patterns that indicate disease
- Distinguish between real abnormalities and artifacts
- Have advanced training in cardiac imaging physics and interpretation
What Happens During a Second Opinion Consultation:
1. Comprehensive Review
- The nuclear cardiologist reviews your ACTUAL images, not just the written report
- They examine the raw data, multiple views, and quantitative measurements
- They correlate findings with your symptoms, risk factors, and other test results
2. Advanced Analysis
- They may apply specialized software analysis not used in the original interpretation
- They compare your images to databases of normal and abnormal scans
- They calculate precise quantitative measures of perfusion and function
3. Expert Interpretation
- They determine if findings represent true disease or artifacts
- They assess the severity and location of any real abnormalities
- They recommend the most appropriate next steps
4. Personalized Guidance
- Should you proceed with catheterization?
- Can you avoid an invasive procedure with additional non-invasive testing?
- What's your actual risk level?
- What should your treatment plan be?
What You Should Bring:
- Original stress test images (not just the report—get the actual CD/DVD of images)
- Complete medical history
- List of all medications
- Recent lab results (cholesterol, blood sugar)
- Any other cardiac testing you've had
- Your questions and concerns written down
The Real Cost-Benefit Analysis: Numbers That Matter
Let's talk money and outcomes—because that motivates clear thinking:
Cost of a Nuclear Cardiology Second Opinion:
- Expert review: ₹15,000 - 35,000
- Virtual consultation (US-based expert): $200 - 400
- Time investment: 1-2 hours
- Total: ₹20,000 - 40,000
Cost of an Unnecessary Catheterization You Could Avoid:
- Cardiac catheterization: ₹50,000 - 1,00,000
- Hospital stay: ₹50,000 - 1,00,000
- Lost work (3-7 days): ₹30,000 - 1,00,000
- Anxiety and psychological impact: Priceless
- Procedure risks and complications: Potentially catastrophic
- Total: ₹1,50,000 - 3,00,000 or MORE
Cost of a Missed Diagnosis That Leads to Heart Attack:
- Emergency treatment: ₹3,00,000 - 8,00,000
- ICU stay: ₹1,50,000 - 3,00,000
- Long-term treatment: ₹20,000 - 50,000 per year for life
- Lost income: ₹2,00,000 - 10,00,000+
- Permanent disability: Priceless loss
- Family impact: Immeasurable
- Total: ₹7,00,000 - 20,00,000+ or DEATH
Do the math. A second opinion is the cheapest insurance policy you'll ever buy.
The Psychology of "But My Doctor Will Be Offended"
I know what you're thinking:
"My cardiologist will be upset if I get a second opinion. It shows I don't trust them."
Let me address this head-on:
Here's the truth about good doctors:
They WELCOME second opinions on complex cases.
Why? Because:
- They know medicine isn't black and white
- They understand their own limitations
- They want what's best for YOU, not their ego
- They recognize that unclear results deserve expert review
Any doctor who gets offended by you seeking a second opinion on inconclusive results is putting their ego above your health.
And that's precisely the kind of doctor you need to run from.
What to say to your current doctor:
"The test results are unclear, and the decision is important. I'd like to get a nuclear cardiology specialist to review the images before we proceed. I value your opinion, and I want to make sure we have all the information before making this decision."
Any reasonable doctor will support this. Period.
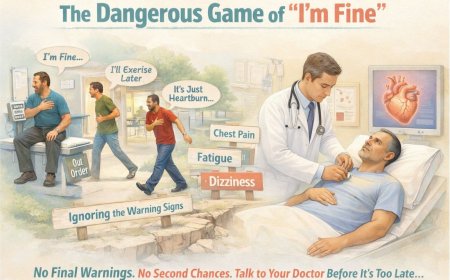
The Hidden Danger: False Reassurance from "Probably Fine"
Here's a mistake that kills people regularly:
Your stress test is equivocal. Your doctor says, "It's probably nothing. Let's just watch it."
You go home relieved. You tell yourself it's fine. You continue ignoring that occasional chest discomfort.
This is called "false reassurance," and it's deadly.
Here's why:
An inconclusive test doesn't mean you're healthy. It means the test couldn't definitively answer the question.
That's completely different from a normal test.
But your brain treats "probably fine" the same as "definitely fine." You stop worrying. You delay further evaluation.
And if there WAS underlying heart disease that the test couldn't quite show clearly—you've just given that disease months or years to progress unchecked.
"Probably fine" isn't good enough when your life is on the line.
The Three Questions to Ask Before ANY Invasive Procedure
If your doctor recommends catheterization based on inconclusive results, ask these three questions:
Question 1: "What is the pre-test probability that I actually have significant coronary disease?"
This forces discussion of your actual risk factors, not just the unclear test result. If you have low overall risk and an equivocal test, an invasive procedure may not be justified.
Question 2: "Are there any additional non-invasive tests that could clarify these results before proceeding to catheterization?"
Options might include:
- Different stress imaging modality (stress echo vs. nuclear)
- CT coronary angiography
- Cardiac MRI
Sometimes a different imaging technique provides the clarity you need without invasive procedures.
Question 3: "Would you recommend a nuclear cardiology specialist review these images before we proceed?"
Watch their reaction carefully. Defensiveness is a red flag. Open consideration is a green flag.
When Time Is NOT on Your Side: The Urgent Scenarios
There are situations where you shouldn't wait for second opinions:
Proceed Immediately to Catheterization If:
-
You have ongoing chest pain or discomfort that's worsening or occurring at rest
- This suggests unstable coronary disease
- Time-sensitive emergency
-
Your stress test showed severely abnormal findings combined with symptoms
- Not truly "inconclusive" at this point
- Risk of heart attack is high
-
You had a positive troponin (heart enzyme) test
- Indicates actual heart muscle damage
- Requires immediate evaluation
-
Your doctor uses words like "unstable angina," "acute coronary syndrome," or "NSTEMI"
- These are medical emergencies
- Second opinions come AFTER stabilization, not before
Seek Second Opinion When:
- You feel fine, but test results are unclear
- You have symptoms, but test results are equivocal
- Two doctors have told you different things
- You're being told you need catheterization "just to be sure"
- Your only "abnormality" is an inconclusive stress test with no symptoms
Trust your instincts. If the recommendation doesn't feel urgent, take time for expert review.
The Virtual Second Opinion Revolution: Accessing World-Class Expertise
Here's something you need to know:
You don't have to be in New York or Boston to get a world-class nuclear cardiology second opinion.
How Virtual Second Opinions Work:
Step 1: Get a copy of your stress test images on CD/DVD (ask your hospital's radiology department)
Step 2: Upload images securely to the specialist's platform
Step 3: Complete a detailed questionnaire about your history and symptoms
Step 4: The nuclear cardiologist reviews everything comprehensively
Step 5: You receive a detailed written report and video consultation explaining findings
Step 6: Armed with expert interpretation, you make an informed decision
Why This Is Game-Changing:
- Access to specialists who interpret 5,000+ nuclear stress tests annually
- No travel required
- Typically faster than waiting for local specialist appointments
- Often more affordable than you'd expect
- Second pair of expert eyes can catch what first review missed
The technology exists. Use it.
What Happens After You Get a Second Opinion: The Path Forward
Scenario 1: Second Opinion Confirms Need for Catheterization
The nuclear cardiologist reviews your images and agrees—you need catheterization.
Now you proceed with confidence:
- You know it's necessary
- You're not wondering "what if?"
- You can mentally prepare
- Your family understands why it's needed
Sometimes the news isn't what you hoped. But certainty is better than uncertainty when making major medical decisions.
Scenario 2: Second Opinion Says You DON'T Need Catheterization
The expert determines the "abnormalities" were artifacts or normal variants. You actually don't have significant coronary disease.
You just avoided:
- Unnecessary invasive procedure
- Significant medical costs
- Physical risks
- Psychological trauma
This is the best-case scenario—and it happens more often than you'd think.
Scenario 3: Second Opinion Recommends Additional Testing First
The expert says: "We need one more test to clarify before deciding about catheterization."
Perhaps:
- CT coronary angiography to directly visualize arteries
- Stress echocardiogram using different imaging modality
- Cardiac MRI for specialized assessment
You get the clarity you need without jumping straight to invasive procedures.
The Questions You're Afraid to Ask (But Need Answers To)
"What if the second opinion disagrees with my doctor? Who do I believe?"
Trust the specialist. A nuclear cardiologist who interprets these specific tests all day has deeper pattern recognition than a general cardiologist who sees all types of heart conditions.
It's like asking: Would you want a general surgeon or a hand surgeon for complex hand surgery? Both are qualified, but one has specialized expertise.
"Will my insurance cover a second opinion?"
Many insurance plans DO cover second opinions, especially when:
- Results are unclear
- Major procedures are being recommended
- Clinical decision-making is complex
Check your policy. Even if not covered, paying out-of-pocket for expert review is worth it.
"What if I'm just being a paranoid, difficult patient?"
You're not paranoid. You're being smart.
Would you buy a house without a proper inspection just because the seller said "trust me"? Would you make a major business investment without due diligence?
Your heart deserves at least as much scrutiny as your financial decisions.
"How do I find a qualified nuclear cardiology specialist?"
Look for:
- Board certification in Nuclear Cardiology
- Certification in Advanced Cardiac Imaging
- Active practice at major cardiac centers
- Experience interpreting thousands of studies annually
- Good communication skills (crucial for explaining complex findings)
Virtual second opinion services connect you with these experts without geography limitations.
The Stark Reality: Your Doctor's Cognitive Biases
Let me share something uncomfortable but important:
Doctors are human. They have cognitive biases that affect their interpretations:
Confirmation Bias
If your doctor suspects you have heart disease, they may interpret unclear findings as "probably abnormal" to confirm their suspicion.
If they think you're low risk, they may interpret the same findings as "probably artifacts."
Neither interpretation may be correct. Expert review removes these biases.
Availability Heuristic
If your doctor recently had a patient with a missed diagnosis, they may be more aggressive in recommending procedures.
If they recently had a patient who had unnecessary catheterization, they may be more conservative.
Your treatment shouldn't depend on what happened to their last patient.
Risk Aversion
Many doctors recommend catheterization for equivocal results because "it's safer to check than to miss something."
While understandable, this approach leads to thousands of unnecessary invasive procedures annually.
A nuclear cardiology expert can determine if "checking" is truly necessary.
The Life-Changing Conversation You Need to Have with Your Spouse
Tonight, before bed, have this conversation with your partner:
"My stress test results are unclear. The doctor wants to do catheterization / the doctor says it's probably fine. But I'm not certain. I want to get a nuclear cardiology second opinion before we make any decisions."
Why This Matters:
Your spouse needs to know:
- That uncertainty exists
- That you're being proactive about clarity
- That you might need their support in getting a second opinion
Don't suffer uncertainty alone. Share the burden.
What Happens If You Do Nothing: The Two Futures
Let me paint two very different pictures of your future:
Future A: You Don't Get a Second Opinion
Scenario A1: You proceed with catheterization that wasn't necessary
- Unnecessary procedure, cost, risk, trauma
- Years of wondering if it was needed
- Medical complications from an avoidable procedure
- Financial burden that wasn't necessary
Scenario A2: You don't get catheterization when you actually needed it
- Silent progression of coronary disease
- Heart attack occurs when disease becomes critical
- Emergency situation instead of planned treatment
- Preventable catastrophe
Both scenarios are BAD. Both are avoidable.
Future B: You Get a Nuclear Cardiology Second Opinion
Outcome B1: Expert confirms need for catheterization
- You proceed with confidence and peace of mind
- Treatment happens at the right time
- You're psychologically prepared
- Family understands and supports you
Outcome B2: Expert determines catheterization isn't necessary
- You avoid unnecessary procedure
- You save money, time, and stress
- You get appropriate monitoring instead
- Peace of mind from expert reassurance
Outcome B3: Expert recommends alternative testing first
- You get clarity without invasion
- Right test at right time
- Informed decision-making
- Optimal pathway forward
Every scenario in Future B is better than every scenario in Future A.
The question is: Which future do you want?
The Action Plan: What to Do
Stop thinking. Stop procrastinating. Here's your step-by-step action plan:
Monday:
-
Call your hospital/clinic where you had the stress test
- Request a copy of your complete stress test images on CD/DVD
- Ask for all reports and documentation
- This usually takes 2-3 business days
-
Research nuclear cardiology second opinion services
- Look for virtual consultation options
- Check qualifications of reviewing physicians
- Compare costs and timelines
- Gather all relevant medical documents:
- Recent lab results (lipid panel, blood sugar)
- List of current medications
- Family history of heart disease
- Previous cardiac testing results
- Written description of any symptoms you're experiencing
- Initiate the second opinion consultation
- Upload your images and documents
- Complete the medical history questionnaire
- Schedule the consultation call/video meeting
-
Have the expert review consultation
- Bring your list of questions
- Take notes or record it (with permission)
- Make sure you understand the findings completely
-
Make your informed decision based on expert interpretation
- Proceed with catheterization if recommended
- Pursue additional testing if suggested
- Continue monitoring if appropriate
- Sleep better knowing you have clarity
The Financial Reality Check: Cost vs. Value
I know you're thinking about money. Let's be completely transparent:
Immediate Costs:
- Second opinion consultation: ₹20,000 - 40,000
What You Potentially Avoid:
If you avoid unnecessary catheterization:
- Procedure cost saved: ₹50,000 - 1,00,000
- Complication risks avoided: Priceless
- Peace of mind: Priceless
- Net Benefit: ₹10,000 - 60,000+
If you catch disease early that was being missed:
- Elective planned treatment vs. emergency treatment: Cost difference of ₹3,00,000 - 10,00,000
- Disability avoided: Priceless
- Life saved: Priceless
- Net Benefit: IMMEASURABLE
The Real Question:
Can you afford NOT to get expert clarity on unclear results that could determine whether you need invasive procedures?
This isn't an expense. It's the best insurance policy you'll ever buy.
The Uncomfortable Truth About Medical Errors
Let me share statistics nobody talks about:
-
The Error Gap: Diagnostic errors occur in up to 1 in 5 medical encounters, affecting millions of patients every year.
-
The Imaging Risk: Misinterpretation of scans is a leading cause of medical error, often resulting in unnecessary procedures or missed treatments.
-
False Alarms: Even advanced tests like Nuclear Stress Tests can have a 15% false positive rate, leading many down a path of invasive surgery they may not need.
-
The Second Opinion Advantage: Research shows that second opinions change or significantly refine the diagnosis in 88% of complex cases
Translation: Getting one opinion—even from a good doctor—isn't enough when results are unclear.
This isn't about not trusting your doctor. It's about:
- Recognizing human limitation
- Acknowledging interpretation challenges
- Seeking specialized expertise when needed
- Protecting yourself from preventable errors
Second opinions aren't paranoia. They're prudence.
Why You're Still Hesitating (And Why You Need to Stop)
Let me address the real reasons you haven't taken action yet:
"I Don't Want to Bother Anyone"
Your health isn't a "bothering." Stop apologizing for advocating for yourself. This is YOUR LIFE.
"I'm Afraid of Finding Out Something Bad"
You're already worried. Clarity—even if it's not what you hoped—is better than living with uncertainty and fear.
"My Doctor Might Think I Don't Trust Them"
A good doctor WANTS you to get expert review on complex cases. If your doctor discourages it, that's a red flag about THEM, not about you.
"It's Too Expensive"
More expensive than an unnecessary catheterization? More expensive than a missed diagnosis leading to heart attack? Really?
"I'll Do It Later"
Your heart disease (if you have it) isn't waiting for "later." Neither should you.
"I'm Too Busy"
You'll have plenty of time during the weeks of recovery from a heart attack. Or the months of recovery from an unnecessary catheterization. Choose your inconvenience wisely.
The Final Word: Your Heart's Message
If your heart could speak right now, here's what it would say:
"I sent you signals. You got tests. The results were unclear.
Now you're at a crossroads.
One path: You take action, get expert clarity, make informed decisions. We work together to protect my health and your life.
Other path: You hope for the best, delay action, and gamble with my function and your future.
I don't gamble. I don't do 'probably fine.' I need definitive answers.
Please. Get that second opinion. Let an expert interpret those unclear findings. Give us both the clarity and protection we deserve.
Because once I suffer permanent damage—from missed disease or unnecessary procedures—I don't fully recover.
This is your moment. Choose wisely. Choose quickly.
Your life literally depends on it."
Take Action NOW
Step 1: Stop reading and start acting
Screenshot this article. Bookmark it. Share it with your spouse.
Step 2: Call for your stress test images TODAY
Don't wait until Monday. Call now and leave a message if needed.
Step 3: Book a second opinion consultation THIS WEEK
Don't delay. Clarity can't wait.
Step 4: Make this a priority
Cancel that optional meeting. Postpone that non-urgent commitment. Your heart comes first.
Expert Second Opinion Resources
Don't navigate this alone. Get expert guidance from nuclear cardiology specialists who interpret thousands of complex stress tests annually.
Assess your cardiac risk and get definitive interpretation of unclear stress test results with a U.S.-based nuclear cardiology specialist.
Connect with experienced U.S.-based heart specialists for a comprehensive second opinion consultation to learn more about your test results.
👉 https://myamericandoctor.com/our-doctors/
You can also enroll in our soon-to-be-launched concierge medical clinic in India, Global Concierge Doctors, which aims to provide US-style primary care services with access to specialized cardiac imaging expertise.
Your unclear test results deserve expert clarity. Get it.
Reader Reflection
Have you ever received inconclusive cardiac test results?
- Yes, and I got a second opinion before making decisions
- Yes, and I proceeded without second opinion (now questioning if I should have)
- Yes, and I'm currently dealing with this situation
- No, but I know someone who has
Share your experience in the comments. Your story might help someone else make a life-saving decision.
Share This Article
Know someone who's been told their stress test is "inconclusive" or "equivocal"?
Someone who's unsure whether they need catheterization?
Share this article with them. It might save them from unnecessary procedures—or catch a diagnosis that could save their life.
Send the direct link.
Sometimes, information from an outside source provides the clarity and courage people need to seek expert review.
The Question That Matters
Do you have clarity about your cardiac status?
Or are you living with the uncertainty of "inconclusive" results, hoping everything will be fine?
That uncertainty could be your biggest risk.
And expert clarity could be your best protection.
The choice is yours. But the clock is ticking.
Written with the hope of preventing unnecessary procedures and catching missed diagnoses. Share it forward.
Related Articles You Should Read:
- Understanding Different Types of Cardiac Stress Tests: Which Is Right for You?
- When to Seek a Cardiologist vs. When to See a Cardiac Imaging Specialist
- The Complete Guide to Cardiac Catheterization: What to Expect
- Non-Invasive vs. Invasive Cardiac Testing: Making the Right Choice
- How to Choose the Right Cardiac Specialist for Your Condition
Your unclear test results aren't "probably fine."
They're definitely unclear.
Get expert clarity. Your life deserves it.
Medical Disclaimer
This article is provided strictly for educational, informational, and awareness purposes only. It is not intended to be, and should not be construed as, professional medical advice, diagnosis, treatment, or a substitute for consultation with qualified healthcare professionals.
No Doctor-Patient Relationship
The information presented in this article does not establish a doctor-patient relationship between the reader and the author, publisher, or any affiliated entities. No medical decisions should be made based solely on the content of this article.
Consult Qualified Medical Professionals
If you are experiencing cardiac symptoms, chest pain, shortness of breath, unexplained fatigue, or any other health concerns mentioned in this article, seek immediate consultation with qualified cardiologists, physicians, or appropriate medical specialists. For medical emergencies, contact emergency services immediately.
Individual Medical Situations Vary
Every person's medical condition, health history, risk factors, and circumstances are unique. Diagnostic tests, treatment options, and medical recommendations must be tailored to individual patients through direct consultation with licensed healthcare providers who have access to complete medical histories and can perform proper clinical evaluations.
Not a Recommendation for Specific Tests or Treatments
References to Cardiac MRI, ECG, stress tests, echocardiograms, or any other diagnostic procedures in this article are for informational purposes only and do not constitute recommendations that you should or should not undergo these tests. All decisions regarding medical testing, diagnosis, and treatment should be made in consultation with qualified healthcare professionals based on your specific medical situation.
No Guarantee of Accuracy or Completeness
While efforts have been made to provide accurate information, medical knowledge continuously evolves. The information in this article may not reflect the most current research, clinical guidelines, or medical practices. The author and publisher make no representations or warranties regarding the accuracy, completeness, or timeliness of the content.
Do Not Disregard or Delay Professional Medical Advice
Never disregard, avoid, or delay obtaining professional medical advice from qualified healthcare providers because of something you have read in this article. If you have questions or concerns about information presented here, discuss them with your personal physician or cardiologist.
Third-Party Resources and Links
Any references to third-party medical services, clinics, doctors, or external websites are provided for informational purposes only and do not constitute endorsements. The author and publisher are not responsible for the content, services, or practices of any third-party entities.
Limitation of Liability
To the fullest extent permitted by law, the author, publisher, and affiliated entities disclaim all liability for any direct, indirect, incidental, consequential, or punitive damages arising from the use of, or reliance on, information contained in this article. This includes, but is not limited to, medical complications, financial losses, or any other adverse outcomes.
Geographic and Regulatory Considerations
Medical regulations, standards of care, insurance coverage, and availability of diagnostic tests vary by country, region, and healthcare system. Information regarding costs, procedures, and medical practices may not be applicable to all geographic locations or healthcare settings.
Your Responsibility
You acknowledge that you are solely responsible for your own health decisions and that you will consult with appropriate licensed healthcare professionals before making any medical decisions or undergoing any diagnostic tests or treatments.
Acknowledgment
By reading and using the information in this article, you acknowledge that you have read, understood, and agreed to this disclaimer in its entirety.
Last Updated: 29th January 2026
For Medical Emergencies: Contact your local emergency services immediately or go to the nearest emergency room.
What's Your Reaction?
 Like
0
Like
0
 Dislike
0
Dislike
0
 Love
0
Love
0
 Funny
0
Funny
0
 Angry
0
Angry
0
 Sad
0
Sad
0
 Wow
0
Wow
0