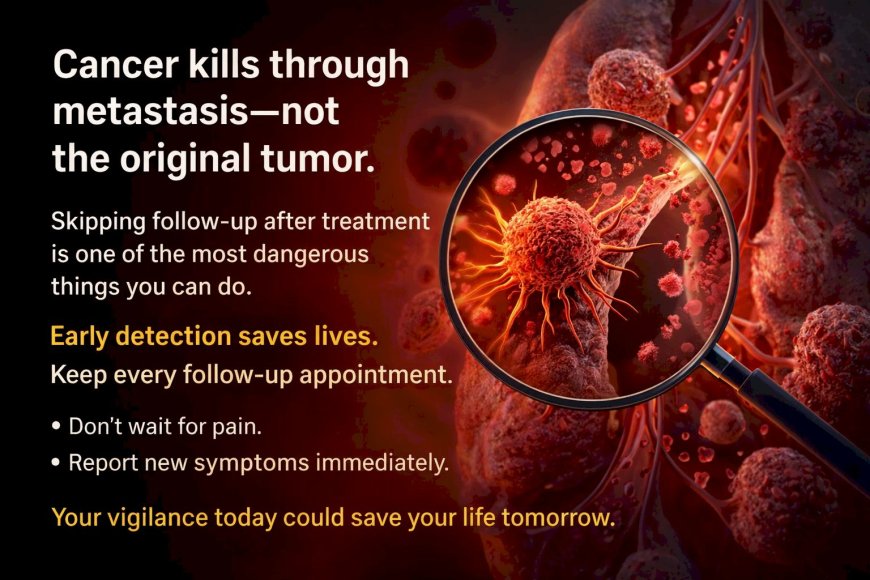
Metastasis: How Cancer Spreads — And Why Understanding It Could Save Your Life
Cancer kills not through the original tumor, but through metastasis — when cancer cells break free, enter your bloodstream or lymphatic system, and colonize distant organs like bones, liver, lungs, and brain. This process happens silently, often without symptoms for months or years. That's why skipping follow-up appointments after cancer treatment is one of the most dangerous decisions you can make. Early detection of metastasis dramatically changes treatment outcomes. Don't wait for pain. Don't assume "cancer-free" means forever. Keep every follow-up. Report new symptoms immediately. Your vigilance today could save your life tomorrow.
At A Glance
Your doctor said "it's spread." Two words that changed everything. Metastasis — the process by which cancer cells break free from where they started and colonize distant organs — is the reason cancer kills. Not the original tumor. Not the lump. The spread. Yet most people have no idea how metastasis works, why it happens, or what they can do to catch it before it reaches the point of no return. This article breaks down the science of how cancer travels through your body, why early detection is your greatest weapon, and what you must do if you or someone you love is at risk.
The Phone Call Nobody Is Ready For
You went for a routine follow-up. Maybe you had a tumor removed months ago. Maybe you finished your chemotherapy and were told things looked "promising." You were starting to breathe again. Starting to believe the nightmare was over.
Then the doctor's expression changed.
"The scans show something in your liver."
Or your lungs. Or your bones. Or your brain.
Your stomach drops. Your ears start ringing. You hear words but they stop making sense.
"The cancer has spread."
Metastasis. The word that turns a fight into a war.
And in many cases, understanding metastasis earlier, knowing the warning signs, and acting faster could have changed this outcome entirely.
So let us explain what is actually happening inside your body when cancer spreads, because this knowledge is not just academic. It could save your life.
What Is Metastasis? (The Truth Behind "It's Spread")
Let us be very direct.
Cancer does not kill most people because of the original tumor. The primary tumor — that lump, that growth, that mass the surgeon removed — is often manageable. Treatable. Even curable.
What kills is metastasis.
Metastasis is the process by which cancer cells leave the primary tumor, travel through your body, and establish new tumors in distant organs. These new tumors are called metastases, and they are made of the same type of cancer cells as the original.
So if breast cancer spreads to your bones, it is not "bone cancer." It is metastatic breast cancer living in your bones. This distinction matters enormously for treatment.
Here is the uncomfortable reality: in many cancers diagnosed at advanced stages, the metastatic process has already begun by the time diagnosis is made. Cancer cells may have been silently traveling through the bloodstream for weeks or months before anyone knew.
And while you were telling yourself "I feel fine," those cells were setting up new colonies in organs you never expected.
How Cancer Spreads: The Step-by-Step Invasion You Cannot Feel
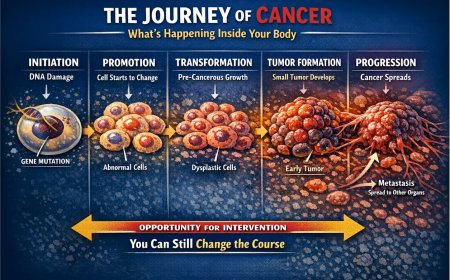
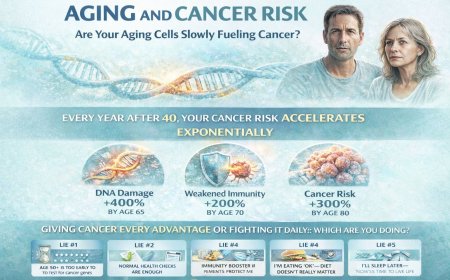
Understanding what happens inside your body during metastasis is not meant to terrify you. It is meant to arm you with knowledge that could change the decisions you make today. The metastatic cascade is a series of well-documented biological steps — five in total — that researchers across the world have studied in remarkable detail.
Step 1: Breaking Free — Local Invasion
Cancer cells in a tumor are held together by proteins and structural elements that act as biological anchors. In a healthy body, cells respect their boundaries. They stay where they belong.
Cancer cells do not.
They produce enzymes — particularly a family called matrix metalloproteinases (MMPs) — that degrade the extracellular matrix and the basement membrane surrounding the tumor. They dissolve structural barriers. They push into healthy tissue around them, a process driven in part by a transformation cancer cells undergo called epithelial-mesenchymal transition (EMT), which makes them more mobile and invasive.
You cannot feel this. There is no pain signal. No warning light. It happens silently, invisibly, at the microscopic level.
What you may be telling yourself: "The tumor hasn't grown much. It's probably stable."
What may actually be happening: Cancer cells at the edges of that tumor are actively breaking through tissue boundaries and preparing to travel.
Step 2: Entering the Highway — Intravasation
Once cancer cells break free from the primary tumor, they need a transportation system. Your body provides two: your blood vessels and your lymphatic system.
Cancer cells push their way into nearby blood vessels or lymph channels — a process called intravasation. Think of it as cancer entering a biological highway system. Once in the circulation, cells can travel to distant parts of the body. Crucially, research has shown that this process is not entirely passive — cancer cells can recruit other cells, including macrophages and platelets, to assist their entry into and survival within the bloodstream.
This is why doctors carefully examine your lymph nodes during cancer staging. Lymph nodes are like checkpoints on the lymphatic highway. If cancer cells are found in nearby lymph nodes, it indicates they have entered the transport system and may already be traveling further.
What you may be telling yourself: "The doctor said the lymph nodes are 'borderline.' That doesn't sound too bad."
The clinical reality: Lymph node involvement signals that cancer may already be in your body's transportation network. This demands urgent investigation and close follow-up with your oncologist.
Step 3: Surviving the Journey — Circulation
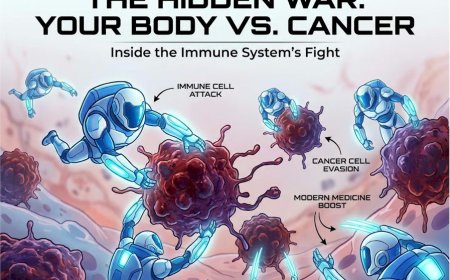
Here is something that surprises many people: most cancer cells that enter the bloodstream actually die.
The circulation is an extremely hostile environment for a cancer cell. Shear forces from blood flow, immune surveillance, and lack of structural support kill the vast majority of circulating tumor cells (CTCs). Research estimates that only approximately 0.01% of circulating tumor cells ultimately form secondary tumors — a testament to how inefficient, yet devastating, the metastatic process is.
But cancer does not need most of them to survive. It only needs a few.
Those survivors have proven they can withstand your body's defenses. Notably, some cancer cells travel in clusters rather than as single cells, and clusters are thought to have a higher metastatic potential than individual cells. Platelets also play a documented role in shielding cancer cells from immune detection during circulation, effectively helping them survive the journey.
What you may be telling yourself: "My immune system is strong. It can handle this."
The clinical reality: Your immune system is fighting, and that is important. But cancer has evolved sophisticated mechanisms to evade immune surveillance — including disguising itself and, in some cases, recruiting immune cells as accomplices. A strong immune system is a vital asset, but it is not an absolute guarantee against metastasis.
Step 4: Finding a New Home — Extravasation
Cancer cells circulating in your bloodstream eventually slow down in the tiny capillary beds of distant organs. They adhere to vessel walls and push their way through the endothelial barrier into the surrounding tissue. This is called extravasation — the reverse of intravasation.
Here is what is both fascinating and clinically significant: cancer does not spread randomly. Different cancers have documented preferred destinations, a phenomenon scientists describe as organotropism.
Breast cancer commonly spreads to bones, lungs, liver, and brain. Lung cancer frequently targets the brain, bones, liver, and adrenal glands. Colon cancer often heads for the liver first, because venous drainage from the colon flows directly to the liver through the portal circulation. Prostate cancer has a well-documented affinity for bone.
This is explained partly by the "seed and soil" theory, first proposed by surgeon Stephen Paget in 1889 and extensively validated by modern molecular research. Cancer cells (seeds) grow best in specific organ environments (soil) because of the chemical signals, growth factors, and cellular architecture those organs provide. Researchers have also identified the concept of the "pre-metastatic niche" — changes that primary tumors induce in distant organs that make those sites more hospitable to incoming cancer cells before they even arrive.
What you may be telling yourself: "If the primary tumor is treated, I'm safe."
The clinical reality: Cancer cells may have left the primary tumor before treatment began. They could be dormant in a distant organ at this very moment, waiting.
Step 5: Colonization — The New Tumor Grows
This is the final and deadliest step.
The cancer cells that survived the journey, escaped the bloodstream, and landed in a new organ now face their biggest challenge: establishing a new tumor in unfamiliar territory.
They need to recruit new blood vessels to feed themselves — a process called angiogenesis. They need to suppress the local immune response. They need to adapt to a completely different tissue environment. Many fail. Some lie dormant for months or even years — microscopic clusters of cells called micrometastases, too small to detect on any scan.
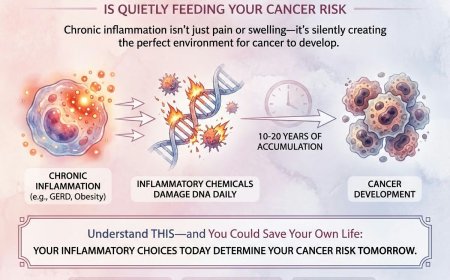
Then, one day, something changes. The exact triggers that reactivate dormant metastatic cells are still an area of active research, but inflammation, immune system changes, and certain cellular signals are thought to play a role. Those dormant cells wake up, begin dividing, and a new tumor appears on a scan that was clear six months ago.
This is why cancer can appear to "come back" years after treatment. Those cells were there all along. Dormant. Waiting.
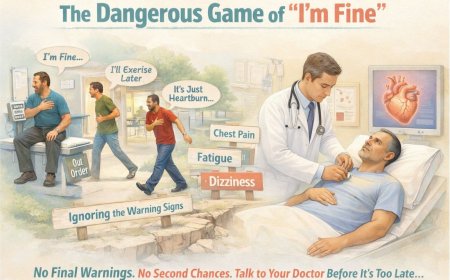
Why Your Brain Does Not Want You to Understand This
If you have read this far, you might feel a tightening in your chest. Fear. Anxiety. A desire to close this article and go watch something on television.
That is your brain doing exactly what it does with threatening information — trying to protect you by encouraging avoidance.
But avoidance is what metastasis thrives on. Delay is its greatest ally.
Every week you postpone a follow-up scan, every month you skip a doctor's appointment because "I feel fine," every test you put off because you are scared of the results — that is time metastasis could be using to establish itself.
Understanding metastasis does not mean living in fear. It means living in awareness. It means knowing WHY your doctor orders those follow-up scans. WHY they monitor your tumor markers. WHY early detection and timely follow-up matter so profoundly.
The American Cancer Society (ACS) and the American Society of Clinical Oncology (ASCO) both publish detailed survivorship care guidelines precisely because the risk of recurrence and metastasis is real and documented. ASCO's survivorship care plans are designed to map out exactly what follow-up monitoring cancer survivors need — and for how long. These plans exist not to keep patients trapped in anxiety, but to catch problems when they are most treatable.
The Warning Signs of Metastasis You Must Not Ignore
Metastasis often announces itself quietly. Here is what to watch for, depending on where cancer has spread:
Bone Metastasis: Deep, persistent pain in your back, hips, ribs, or limbs that does not respond to usual pain relief. Pain that is worse at night or at rest. Bones that fracture with minimal or no trauma — a condition called a pathological fracture. Hypercalcaemia (elevated calcium from bone breakdown) can also occur and may cause nausea, confusion, and fatigue.
What you may be telling yourself: "I'm getting older. Everyone has back pain. It's probably arthritis."
The clinical reality: Persistent, unexplained bone pain — especially if you have a cancer history — requires investigation. A bone scan or imaging can provide answers quickly.
Liver Metastasis: Unexplained fatigue. Loss of appetite. Nausea. Pain or fullness in the upper right abdomen. Unexplained weight loss. Yellowing of the skin or eyes (jaundice) is a later sign indicating significant liver involvement.
What you may be telling yourself: "I've been stressed and not eating well. The fatigue is probably from work."
The clinical reality: The liver is a resilient organ that can harbor significant disease before symptoms appear. If you have a cancer history and notice these changes, contact your oncologist promptly.
Lung Metastasis: A cough that persists beyond three weeks without explanation. Shortness of breath with activities that did not bother you before. Chest pain. Coughing up blood, even in small amounts.
What you may be telling yourself: "It's the pollution. Everyone coughs. It's allergy season."
The clinical reality: A persistent cough in someone with a cancer history warrants investigation. Do not let familiarity with environmental factors blind you to something that requires medical attention.
Brain Metastasis: New headaches — particularly ones that are worse in the morning or that wake you from sleep, as these can reflect increased intracranial pressure. New vision changes, balance problems, confusion, personality changes, or weakness in limbs. Seizures in someone who has never had them before.
What you may be telling yourself: "It's just stress. I've been working too hard. I need more sleep."
The clinical reality: New neurological symptoms in anyone with a cancer history require prompt medical evaluation. Do not wait.
Real Stories That Should Move You to Action
Story: Amit, 52, Gurugram
Amit had a colon tumor removed two years ago. Stage 2. The surgeon said margins were clear. Follow-up was recommended every six months.
Amit attended one follow-up. Felt well. Decided the rest were unnecessary.
"I'd beaten cancer. Why keep going back? The tests are expensive and stressful."
Eighteen months later, persistent fatigue brought him back to the doctor. Scans revealed multiple liver metastases. What had been curable Stage 2 colon cancer was now Stage 4 metastatic disease.
His words: "One follow-up scan might have caught this when it was a tiny spot on my liver. One scan. I skipped it because I was scared of hospitals and wanted to forget. Now I can't forget."
Story: Meera, 45, Mumbai
Meera completed treatment for breast cancer — surgery, chemotherapy, everything. Declared cancer-free. She celebrated. She moved on.
Two years later, persistent lower back pain appeared. She attributed it to long office hours and tried physiotherapy for three months.
When the pain worsened, she finally saw her oncologist. A bone scan revealed metastatic breast cancer in her spine and pelvis.
Her words: "I thought cancer-free meant forever. Nobody clearly explained that cancer cells could have been hiding in my bones for two years. If I had connected back pain to my cancer history sooner, if I had gone to my oncologist instead of a physiotherapist first, treatment could have started months earlier."
The "I've Beaten Cancer" Trap
Let us address something that many cancer survivors do not fully understand:
"Cancer-free" after treatment does not mean cancer is permanently gone from your body.
It means scans and tests cannot detect cancer at that moment. It means treatment has been successful to the extent that current medical technology can measure. This is genuinely wonderful news. It deserves to be celebrated.
But microscopic cancer cells — too small for any scan to detect — may still exist in your body. This is precisely why oncologists schedule follow-up appointments for months and years after treatment. Not to keep you anchored in the identity of "cancer patient" indefinitely. But because catching a recurrence or early metastasis dramatically improves the range of treatment options available to you.
The ACS and ASCO have developed formal survivorship care plans for exactly this reason. These plans differ by cancer type, stage, and treatment received, and outline recommended follow-up schedules, surveillance tests, and lifestyle factors. Asking your oncologist about your specific survivorship care plan is one of the most important conversations you can have after completing cancer treatment.
The Excuses That Cost Lives
Excuse #1: "My cancer was caught early. I don't need to worry about metastasis."
Early-stage cancers carry a much lower risk of metastasis, but the risk is not zero. Some aggressive cancer subtypes can spread even from small, early-stage tumors. Follow-up is not optional regardless of your stage at diagnosis.
Excuse #2: "I feel completely fine. If cancer had spread, I'd know."
Metastasis can be entirely silent for months or even years. Micrometastases produce no symptoms. By the time you "feel" something has changed, the disease may be significantly advanced. Scans and blood tests can detect what your body cannot yet signal.
Excuse #3: "The follow-up appointments and tests are too expensive."
The financial reality of cancer care is genuine and should not be dismissed. If cost is a barrier, speak openly with your oncologist about which tests are most clinically critical for your specific situation. Many government hospitals in India offer subsidized cancer follow-up care. Charitable organizations can assist with costs. Some cancer types require less frequent or less expensive surveillance than others. Work with your medical team to find a follow-up plan that is both medically sound and practically achievable. Skipping follow-up entirely, however, is a risk that carries consequences far greater than financial ones.
Excuse #4: "I'll try Ayurveda or other alternative therapies instead of going back to the oncologist."
Alternative and complementary therapies may support your overall wellbeing, and many patients discuss these openly with their doctors. However, no alternative therapy can detect metastasis. No herbal preparation, no homeopathic remedy, no supplement can replace imaging, blood tests, or oncological surveillance. Using alternative medicine as a substitute for cancer follow-up is not a wellness choice. It is a medically dangerous decision.
Excuse #5: "I don't want to live in fear of cancer forever."
This is the most understandable concern of all. Cancer fatigue is real. Scan anxiety — sometimes called "scanxiety" — is a documented psychological experience among survivors. The desire to move on with life is completely human and completely valid.
But here is the reframe: follow-up is not living in fear. It is taking control. It is telling cancer that it does not get to surprise you. Psychological support, including counseling, support groups, and mindfulness practices, can help survivors manage the anxiety of follow-up without abandoning it. Your oncology team can refer you to appropriate support resources.
What You Can Actually Do
Understanding metastasis is not about helplessness. It is about empowerment.
If you are currently in cancer treatment: Complete your treatment as prescribed. Do not skip sessions or stop early because you feel better. The treatment protocol exists to maximize your chances of eliminating or controlling cancer cells — including any that may be attempting to spread.
If you have finished cancer treatment: Keep every follow-up appointment. Ask your oncologist specifically about your survivorship care plan — what tests are recommended, at what intervals, and for how long. Both ACS and ASCO provide cancer-specific survivorship guidelines that your doctor can reference. If cost is a genuine barrier, have that conversation directly with your care team. But do not skip follow-ups silently.
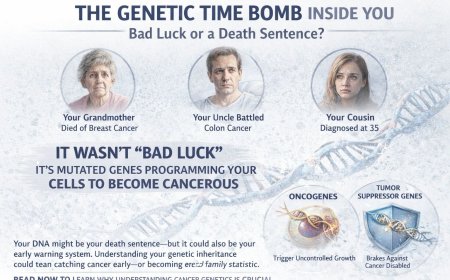
If you have a family history of cancer: Understand your risk. Discuss genetic testing with your doctor if multiple family members have had cancer, particularly at young ages. Start recommended screenings on time — or earlier if your doctor advises based on your personal risk profile. The ACS provides screening guidelines for breast, colorectal, lung, prostate, and cervical cancer, among others, which can help you know when to start and how often to screen.
If you notice new symptoms after cancer treatment: Do not explain them away. Do not wait weeks to see whether they resolve on their own. Contact your oncologist. Describe what you are feeling. Let your medical team determine whether investigation is warranted.
Persistent bone pain. Unexplained weight loss. A cough that will not go away. Unusual fatigue. New headaches. Any of these in someone with a cancer history warrants a phone call to your doctor — not next month, not next week. Now.
What You Should Do in the Next 48 Hours
If you are a cancer survivor and have missed follow-up appointments:
- Call your oncologist's office today and schedule what is overdue
- Write down any new symptoms you have been dismissing — even ones that seem minor
- Tell a family member about your appointment so they can help hold you accountable
- Show up — do not cancel
If you have unexplained symptoms and a cancer history:
- Do not spend the night searching your symptoms online
- Call your oncologist first — not your general physician, not a physiotherapist, not a practitioner of alternative medicine
- Be entirely honest about what you are experiencing and for how long
- Follow through on every test your doctor recommends
If you love someone who has had cancer:
- Ask them — gently but clearly — whether they are keeping up with their follow-up care
- Offer to go with them to appointments
- Watch for symptoms they may be minimizing or hiding
- Share this article with them
Professional Support Options
If you are experiencing possible cancer symptoms, seeking a second opinion, or unsure which tests or treatments are right for you, do not wait. Speak with a qualified oncologist today.
Connect with experienced U.S.-based cancer specialists for a comprehensive second-opinion consultation. They will carefully review your case and help determine the most appropriate next steps for your individual health needs:
You may also choose to enroll in our upcoming concierge medical clinic in India, Global Concierge Doctors. We offer U.S.-style primary care with 24/7 access to India-based physicians for ongoing guidance on any health concern. When required, we coordinate referrals to trusted specialists in India and the U.S. for advanced evaluation and care.
Your health decisions today shape your life tomorrow.
The Final Word: Cancer's Greatest Weapon Is Your Silence
Metastasis does not announce itself with sirens and flashing lights. It moves quietly. Patiently. While you are busy living, it is busy traveling.
But here is what metastasis cannot overcome: a patient who shows up. A patient who keeps their follow-up appointments. A patient who refuses to ignore new symptoms. A patient who understands that "cancer-free" is a gift that requires ongoing vigilance to protect.
Your body has been through a war. Do not abandon the watchtower just because the battlefield is quiet.
Stay vigilant. Stay informed. Stay alive.
Reader Poll
Are you keeping up with your cancer follow-up appointments?
- [ ] Yes, I never miss one
- [ ] I've skipped a few but I'm scheduling one now
- [ ] I stopped going — but this article is changing my mind
- [ ] I'm newly diagnosed and learning about metastasis for the first time
Share This Article
Know someone who finished cancer treatment and stopped going for follow-ups?
Know someone dismissing new symptoms because "I beat cancer already"?
Share this article. Understanding metastasis saves lives. Silence and avoidance cost them.
Summary
Metastasis — the spread of cancer from its original site to distant organs — is responsible for the majority of cancer-related deaths. Cancer cells break free from tumors through a process of local invasion, enter the bloodstream or lymphatic system via intravasation, circulate through the body, and colonize organs such as bones, liver, lungs, and brain through extravasation and colonization. This entire process can unfold silently, with no symptoms, for months or even years. Understanding how metastasis works empowers patients and survivors to prioritize follow-up care, recognize warning signs early, and take immediate action when new symptoms appear. Early detection of metastasis significantly improves the treatment options available. Structured survivorship care plans, as recommended by the American Cancer Society and the American Society of Clinical Oncology, exist precisely to catch recurrence and spread at the earliest and most treatable stage. Your vigilance after cancer treatment is not optional. It is lifesaving.
Medical Disclaimer
This article is provided strictly for educational, informational, and awareness purposes only. It is not intended to be, and should not be construed as, professional medical advice, diagnosis, treatment, or a substitute for consultation with qualified healthcare professionals.
No Doctor-Patient Relationship
The information presented in this article does not establish a doctor-patient relationship between the reader and the author, publisher, or any affiliated entities. No medical decisions should be made based solely on the content of this article.
Consult Qualified Medical Professionals
If you are experiencing any symptoms mentioned in this article, have been diagnosed with cancer, or have concerns about cancer risk, seek immediate consultation with qualified oncologists, physicians, or appropriate medical specialists. For medical emergencies, contact emergency services immediately.
Individual Medical Situations Vary
Every person's medical condition, health history, risk factors, cancer type, and circumstances are unique. Diagnostic tests, treatment options, and medical recommendations must be tailored to individual patients through direct consultation with licensed healthcare providers who have access to complete medical histories and can perform proper clinical evaluations.
Not a Recommendation for Specific Tests or Treatments
References to biopsies, imaging studies (CT scans, PET scans, MRI), blood tests, tumor markers, chemotherapy, radiation therapy, immunotherapy, targeted therapy, surgery, or any other diagnostic procedures and treatments in this article are for informational purposes only and do not constitute recommendations that you should or should not undergo these tests or treatments. All decisions regarding medical testing, diagnosis, and treatment should be made in consultation with qualified healthcare professionals based on your specific medical situation.
No Guarantee of Accuracy or Completeness
While every effort has been made to provide accurate and current information, medical knowledge evolves continuously, particularly in the rapidly advancing field of oncology. The information in this article may not reflect the most current research, clinical guidelines, treatment protocols, or medical practices at the time of reading. The author and publisher make no representations or warranties regarding the accuracy, completeness, or timeliness of the content.
Do Not Disregard or Delay Professional Medical Advice
Never disregard, avoid, or delay obtaining professional medical advice from qualified healthcare providers because of something you have read in this article. If you have questions or concerns about information presented here, discuss them with your personal physician or oncologist. Early detection and prompt treatment significantly improve cancer outcomes.
Third-Party Resources and Links
Any references to third-party medical services, clinics, doctors, cancer centres, or external websites are provided for informational purposes only and do not constitute endorsements. The author and publisher are not responsible for the content, services, or practices of any third-party entities.
Limitation of Liability
To the fullest extent permitted by law, the author, publisher, and affiliated entities disclaim all liability for any direct, indirect, incidental, consequential, or punitive damages arising from the use of, or reliance on, information contained in this article. This includes, but is not limited to, medical complications, treatment decisions, financial losses, or any other adverse outcomes.
Geographic and Regulatory Considerations
Medical regulations, standards of care, availability of diagnostic tests, treatment protocols, and access to cancer therapies vary by country, region, and healthcare system. Information regarding procedures and medical practices may not be applicable to all geographic locations or healthcare settings.
Clinical Trials and Experimental Treatments
Any references to clinical trials, experimental treatments, or investigational therapies are for informational purposes only. Participation in clinical trials should only be considered after thorough discussion with your oncology team and full understanding of all associated risks and benefits.
Your Responsibility
You acknowledge that you are solely responsible for your own health decisions and that you will consult with appropriate licensed healthcare professionals before making any medical decisions or undergoing any diagnostic tests or treatments.
Acknowledgment
By reading and using the information in this article, you acknowledge that you have read, understood, and agreed to this disclaimer in its entirety. You further acknowledge that this article has been created with the assistance of artificial intelligence. While every effort has been made to ensure accuracy, AI-generated content may occasionally contain errors, omissions, or inaccuracies. The information presented here is intended solely for educational and informational purposes and should not be relied upon as a substitute for professional medical advice. Readers are strongly encouraged to consult qualified healthcare professionals, refer to peer-reviewed medical literature, and cross-reference information from established clinical sources before making any health-related decisions.
Last Updated: 7th February 2026
What's Your Reaction?
 Like
0
Like
0
 Dislike
0
Dislike
0
 Love
0
Love
0
 Funny
0
Funny
0
 Angry
0
Angry
0
 Sad
0
Sad
0
 Wow
0
Wow
0