Non-Small Cell Lung Cancer (NSCLC): What Every Indian Needs to Know Right Now
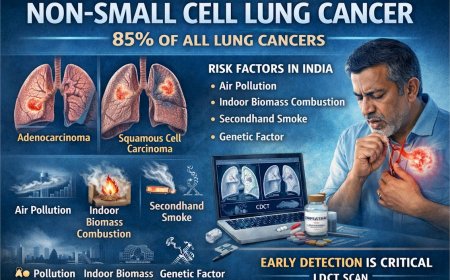
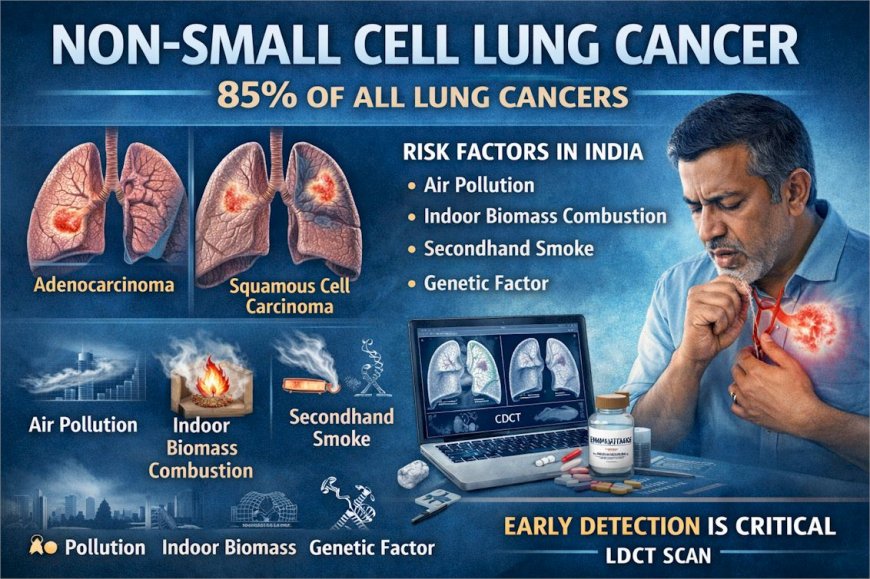
Non-Small Cell Lung Cancer is the most common form of lung cancer, accounting for approximately 85% of all cases globally. Its three main subtypes — adenocarcinoma, squamous cell carcinoma, and large cell carcinoma — differ in biology, location, and treatment approach. In India, between 40 and 50% of lung cancer patients are non-smokers, making air pollution, indoor biomass combustion, secondhand smoke, and genetic factors critically important risk factors for the Indian population. Early-stage NSCLC is typically asymptomatic; by the time symptoms are undeniable, the cancer has often advanced. The updated 2023 ACS guideline now recommends annual LDCT screening for current and former smokers aged 50–80 with a 20+ pack-year history, with no quit-year restriction. Comprehensive molecular and biomarker testing before treatment is essential. Modern treatment including targeted therapy, immunotherapy, and surgery offers meaningful hope — but early detection determines the options available.
At A Glance
That cough has been with you for six weeks. You blamed the Delhi pollution. Then the weather change. Then an old cold that never fully resolved. You feel mostly fine otherwise — which is exactly what makes Non-Small Cell Lung Cancer so dangerous. NSCLC grows quietly, often without pain or dramatic symptoms, while most people are busy finding sensible explanations for what their body is telling them. This article cuts through the denial, explains what NSCLC actually is, who is truly at risk in India (the answer will surprise you), what the latest guidelines say about screening and treatment, and what you must do if even one warning sign sounds familiar.
The Cough You Are Still Explaining Away
It started in October. A dry cough that sat in your chest and would not leave. You bought lozenges, then a cough syrup, then an antibiotic from the neighbourhood pharmacy. The cough softened slightly, then returned. Some mornings you woke up short of breath climbing to the second floor — but your building has no lift, you are getting older, and Delhi's air that week was reading 380 on the AQI. Reason enough, you told yourself.
You have not mentioned it to a doctor.
Here is the uncomfortable reality: a persistent cough lasting more than three weeks, particularly in anyone over 40 living in a high-pollution urban environment, is one of the most important warning signals the lungs can produce. India's oncologists see this pattern every day — a patient who waited six months to seek evaluation, whose scan now shows a mass that was almost certainly there when the cough first began.
The waiting did not make the tumour smaller. It gave it time.
What Is Non-Small Cell Lung Cancer?
Lung cancer is divided into two broad categories. Small Cell Lung Cancer accounts for roughly 15% of cases and is strongly linked to heavy tobacco use. Non-Small Cell Lung Cancer constitutes 85% of cases, comprising predominantly lung adenocarcinoma and squamous cell carcinoma. NSCLC is not a single disease — it is an umbrella term for three distinct subtypes, each with different biology, behaviour, and treatment implications.
Adenocarcinoma is the most common subtype globally and in India. It is the most common and often occurs in the outer parts of the lung, frequently affecting non-smokers and younger people. Because it develops in the lung's periphery away from the major airways, it may grow for months or longer before causing noticeable symptoms — which is precisely why it is so often found at an advanced stage.
Squamous Cell Carcinoma usually develops in the central parts of the lungs and is closely linked to smoking. Because of its central location near the bronchi, it tends to cause respiratory symptoms — cough, wheezing, and blood-tinged sputum — somewhat earlier in its course than adenocarcinoma.
Large Cell Carcinoma is the least common of the three, can arise anywhere in the lung, and tends to grow and spread more rapidly. It is often diagnosed only after it has reached an advanced stage.
Knowing your subtype is not academic. It directly determines which treatments your oncologist will recommend and whether you may benefit from the new generation of targeted oral therapies that have transformed outcomes for many patients.
The India-Specific Reality: This Is Not Only a Smoker's Disease
Let's address the most dangerous assumption about lung cancer in India directly.
You do not have to smoke to get NSCLC.
A substantial proportion of persons with lung cancer in Southeast Asia are never-smokers: between 40 and 50% in studies from India, and 83% in South Asian women. Read that again. In India, depending on the study and the centre, between four and five out of every ten lung cancer patients have never smoked a cigarette in their lives.
In a large north Indian study, nearly 44 per cent of new lung cancers were noted in non-smokers.
This is not a coincidence. It is a consequence of the environment in which millions of Indians live and breathe.
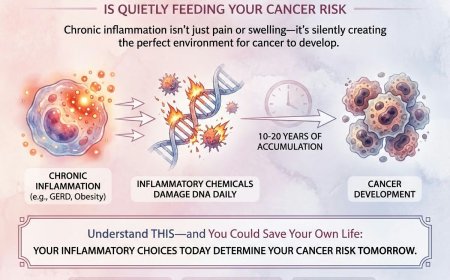
Long-term exposure to particulate matter can trigger mutations in lung cells, leading to uncontrolled cell growth. The International Agency for Research on Cancer (IARC) has classified outdoor air pollution — and PM2.5 particulate matter specifically — as a Group 1 human carcinogen. Delhi and several other Indian cities consistently record PM2.5 levels that exceed safe limits by multiples, not fractions.
Indoor air pollution, occupational exposures to asbestos, silica and diesel exhaust, rapid urbanisation with associated air quality deterioration, and possible genetic predispositions unique to the Indian population further explain the rising burden of adenocarcinoma, especially in non-smokers.
The practical implication for you, reading this in Delhi or Mumbai or Bengaluru or Chennai: if you have been telling yourself that lung cancer is not your concern because you don't smoke, that assumption may be costing you the early detection window that changes outcomes.
Who Is At Risk: The Full Picture
Tobacco use remains the single largest risk factor globally. This includes cigarettes, bidis, cigars, hookah, and pipe tobacco. The longer someone smokes and the more heavily they smoke, the higher the risk. Former smokers remain at elevated risk for years after quitting — the risk declines gradually but never fully returns to non-smoker baseline.
Secondhand smoke is a clinically established risk factor. Environmental tobacco smoke exposure during childhood is strongly associated with the risk of developing lung cancer. For women in rural and urban India, indoor exposure to tobacco smoke from family members is a significant contributor.
Air pollution. Fine particulate matter (PM2.5) is linked to higher rates of lung cancer, especially in urban areas with heavy traffic and industrial activity. For residents of India's most polluted cities, this is not a theoretical future risk — it is an ongoing daily exposure.
Indoor biomass fuel combustion. Research from AIIMS Bhubaneswar published in 2024 found significant associations between high-risk occupations, indoor biomass use without proper ventilation, low BMI, and family history of lung cancer in non-smoking lung cancer patients. Women who cook over open biomass fires in poorly ventilated kitchens are at meaningfully elevated risk.
Radon gas. Radon gas, a naturally occurring radioactive gas found in soil and building materials, is the second leading cause of lung cancer after smoking. Awareness of radon as a residential hazard is still limited in India but is growing among thoracic oncologists.
Occupational exposures to asbestos, arsenic, chromium, nickel, and diesel exhaust are established risk factors for workers in construction, mining, manufacturing, and related industries.
Family history and genetics. Having a first-degree relative with lung cancer increases your risk. Certain genetic variations and mutations, like those in the p53 tumour suppressor gene, are associated with a higher risk of NSCLC.
Prior lung disease. Chronic obstructive pulmonary disease (COPD) and pulmonary fibrosis both independently increase lung cancer risk, beyond what tobacco alone would explain.
Sound familiar? Even two of these factors together place you in a category where a conversation with your doctor about lung health is not excessive caution — it is common sense.
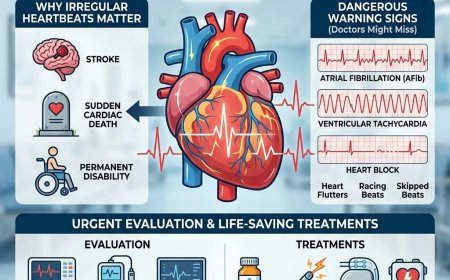
Recognising the Warning Signs
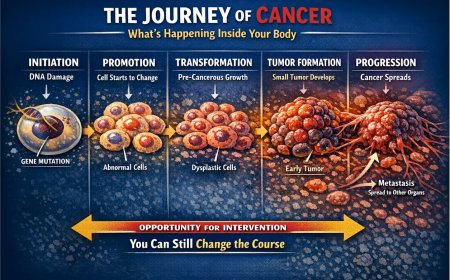
NSCLC in its early stages is frequently asymptomatic or produces only mild symptoms that are easily attributed to other causes. This is not because the disease is not present. It is because the outer regions of the lung where adenocarcinoma typically arises have no pain receptors in the way the skin or digestive tract does. A tumour can establish itself, develop its own blood supply, and begin to grow without producing any sensation the patient can localise or describe as alarming.
By the time symptoms become impossible to dismiss, the cancer has often already spread beyond the primary site.
Here is what to watch for — and take seriously:
A persistent cough that is new, progressively worsening, or simply will not resolve over three or more weeks deserves medical evaluation. This is especially true if you are over 40, have any smoking or secondhand smoke exposure history, or live in a high-pollution environment.
Coughing up blood or blood-streaked sputum — even once, even a small amount — should never be dismissed as a nosebleed or dry throat. It requires prompt medical evaluation without delay.
Unexplained breathlessness that is new or progressively worsening, without a clear explanation such as known heart disease or asthma, deserves investigation.
Persistent chest pain that worsens with deep breathing, coughing, or laughing can indicate that a tumour has grown to involve the chest wall or the pleural lining of the lungs.
Unexplained hoarseness lasting more than a few weeks, particularly when not associated with a throat infection, can result from a tumour pressing on the recurrent laryngeal nerve that controls the vocal cord.
Unexplained weight loss — losing weight without trying and without any obvious cause — is one of the most important and clinically significant general warning signs of cancer.
Persistent fatigue that is disproportionate to your activity level and is not explained by poor sleep, anaemia, or stress alone.
Recurring respiratory infections — pneumonia or bronchitis that keeps returning or unusually resists treatment — can occur when a tumour partially obstructs an airway, allowing secretions to pool and become infected.
Bone pain, particularly in the back, hips, or ribs, and neurological symptoms including headaches, seizures, vision changes, or unexplained weakness can indicate that NSCLC has spread to bones or the brain. These are signs of advanced disease.
If any of these symptoms have persisted for more than two to three weeks without a clear explanation, that is sufficient reason to see a doctor. Not next month. This week.
Why Your Brain Is Not Helping You Right Now
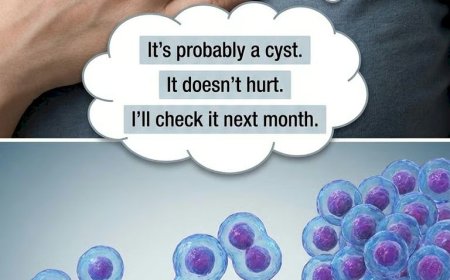
Here is what no one says plainly enough: the human mind is extraordinarily skilled at explaining away symptoms that frighten it.
A cough that has been present for six weeks gets attributed to pollution, season change, an old cold, dry weather. Breathlessness climbing stairs gets attributed to ageing, stress, weight gain. Blood in sputum gets rationalised as a burst blood vessel or a throat scratch. Every explanation feels reasonable. Every explanation delays the appointment that could change the outcome.
What you're telling yourself: "I don't smoke. Lung cancer wouldn't happen to me."
The reality: Between 40 and 50% of lung cancer patients in Indian studies are non-smokers. Adenocarcinoma, the most common subtype, disproportionately affects non-smokers — particularly women and those with prolonged indoor or outdoor air pollution exposure. Smoking reduces your risk substantially. It does not reduce it to zero, and it does not protect against pollution-driven or genetically influenced disease.
What you're telling yourself: "I'd know if it was serious. I'd feel sicker."
The reality: Early-stage NSCLC is frequently asymptomatic or produces only mild, easily explained symptoms. Feeling "mostly fine" is entirely consistent with a lung tumour that has not yet obstructed major airways or spread to other organs. In fact, feeling mostly fine is exactly when you want to find it — because at that stage, the most effective treatments are available.
What you're telling yourself: "I'll wait and see if the cough gets worse."
The reality: Waiting benefits the tumour, not you. The five-year relative survival rate varies markedly for patients diagnosed at local stage (64%), regional stage (36%), or distant stage (9%). The difference between those numbers is, in large part, the time between the first symptom and the first appointment.
What you're telling yourself: "I'll go after this project / this month / this season."
The reality: Cancer does not adjust its timeline to yours. A CT scan takes thirty minutes. The consequences of not booking one can last a lifetime.
A Story Worth Hearing
Meera was 48 years old, a non-smoker who had lived in Delhi for over twenty years. She worked in a school and was known for her energy and reliability. She developed a cough in winter — nothing unusual in Delhi in December — and took a course of antibiotics. The cough eased, then returned in February. By March, she noticed she was getting slightly breathless taking the stairs in her building. She put it down to the fact that she had been less active.
She told herself it was stress. She told herself it was the pollution. She told herself she would see the doctor after her daughter's board exams were over.
By the time she walked into a pulmonologist's office in June — seven months after the cough began — her CT scan showed a 5-centimetre mass in the left lower lobe with enlarged mediastinal lymph nodes. The biopsy confirmed Stage 3A adenocarcinoma.
Biomarker testing revealed an EGFR mutation — which meant she was eligible for targeted oral therapy. She is currently on treatment, managing reasonably well.
But her oncologist was direct with her: "If you had come when the cough began, this was almost certainly Stage 1 or early Stage 2. The surgery would have been curative. We are now managing a much more complex situation."
Seven months of sensible-sounding explanations for a cough she already knew was not normal.
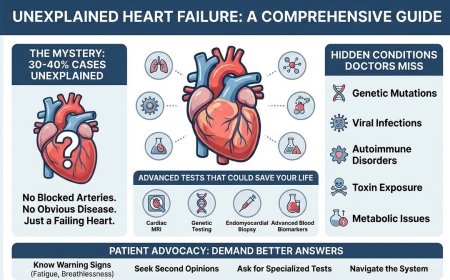
How NSCLC Is Diagnosed: What to Expect
If a doctor suspects lung cancer based on your symptoms and history, the evaluation typically follows a structured path.
Imaging is the first step. A chest X-ray may reveal an abnormality, though small peripheral tumours can be missed. A CT scan of the chest provides far more detailed information — the size, location, and characteristics of any mass, and whether lymph nodes appear enlarged. If initial imaging raises concern, a PET-CT scan may be performed to assess metabolic activity and whether cancer has spread to other regions of the body.
Biopsy is essential to confirm the diagnosis and identify the precise subtype of NSCLC. This may be done via bronchoscopy (a thin camera passed into the airways), CT-guided needle biopsy through the chest wall, or biopsy of accessible lymph nodes. The tissue sample is examined by a pathologist to confirm the cancer type and guide further testing.
Molecular and biomarker testing is now a critical component of NSCLC diagnosis and cannot be omitted. Molecular diagnostics now play a pivotal role in guiding treatment strategies, with actionable genomic alterations informing the use of EGFR, ALK, ROS1, KRAS, NRG1, and other targeted inhibitors in both early and advanced settings. For the Indian patient, this is particularly important: EGFR mutations occur in approximately 23 to 30% of lung adenocarcinoma cases in India — a higher frequency than in Western populations — meaning a significant proportion of Indian NSCLC patients may be eligible for effective targeted oral therapy. PD-L1 expression testing guides immunotherapy decisions. Asking your oncologist specifically about comprehensive molecular and biomarker testing before any treatment decision is made is not only appropriate — it is medically essential.
Staging determines how far the cancer has spread and is the foundation for all treatment decisions. NSCLC is staged using the TNM (Tumour-Node-Metastasis) system, resulting in Stage 1 through Stage 4 classifications. Stage 1 indicates a localised tumour confined to the lung. Stage 4 indicates spread to distant organs. The IASLC has recently developed the 9th edition of NSCLC staging, with key modifications including reclassification of stage groups based on a more refined nodal category and more nuanced metastatic descriptors that better distinguish distinct patterns of metastatic spread.
A brain MRI is often performed as part of staging for NSCLC, as the brain is a relatively common site of spread in certain subtypes.
Treatment: What Modern Medicine Now Offers
The treatment of NSCLC has been transformed more dramatically in the past decade than in the preceding forty years. A diagnosis of NSCLC in 2025 is a medically different situation from what it was even ten years ago — not because the biology has changed, but because the therapeutic tools available to treat it have.
Surgery remains the primary treatment for early-stage NSCLC (Stage 1 and Stage 2, and selected Stage 3 cases) where the tumour can be completely removed and the patient's lung function is sufficient. If you have Stage 1 NSCLC, surgery may be the only treatment you need. Surgery will either remove the lobe of the lung that has the tumour (lobectomy) or remove a smaller piece of the lung (sleeve resection, segmentectomy, or wedge resection). Minimally invasive approaches including video-assisted thoracoscopic surgery (VATS) are increasingly used at high-volume thoracic surgery centres.
Adjuvant therapy after surgery has become an important component of early-stage management. For people with Stage 1 NSCLC that has a higher risk of coming back based on size, location, or other factors, chemotherapy, immunotherapy, and possibly targeted therapy such as alectinib or osimertinib after surgery may lower the risk that cancer will return.
Chemotherapy based on platinum doublet regimens remains an important part of NSCLC treatment — as adjuvant therapy after surgery, in combination with radiation for locally advanced disease, and as systemic therapy in Stage 4.
Targeted therapy is one of the most significant advances in NSCLC management. Targeted therapies are increasingly being integrated into early-stage management, with adjuvant osimertinib for EGFR-mutated NSCLC and alectinib for ALK-positive NSCLC demonstrating substantial survival benefits. For eligible patients with EGFR mutations, ALK rearrangements, ROS1 rearrangements, and other actionable alterations, targeted oral medications are often more effective and better tolerated than traditional chemotherapy, and represent the standard of care per current NCCN and ASCO guidelines.
Radiation therapy is used in multiple contexts: as concurrent treatment with chemotherapy for unresectable Stage 3 disease, as stereotactic body radiation therapy (SBRT) for early-stage patients unsuitable for surgery, and as palliative treatment for symptom control in advanced disease.
Immunotherapy — checkpoint inhibitors that target the PD-1/PD-L1 pathway — has produced durable responses in subsets of NSCLC patients and is now integrated across multiple stages of disease. For Stage 3 unresectable NSCLC treated with concurrent chemoradiation, durvalumab maintenance immunotherapy is now standard of care per ASCO and NCCN guidelines, based on Phase 3 trial data.
Since 2024, the NSCLC landscape has undergone a transformative shift, driven by 11 FDA approvals, with recent advances in molecular profiling, targeted therapies, and immunotherapies revolutionising NSCLC management and ushering in an era of personalised treatment with improved patient outcomes.
The fundamental point: modern oncology has more effective tools for NSCLC than at any prior point in history. Those tools work best — and in some cases only — when the cancer is found early and when comprehensive biomarker testing has been performed before treatment decisions are made.
Lung Cancer Screening: The Updated ACS Guidelines You Need to Know
For individuals at elevated risk due to smoking history, the evidence supporting low-dose CT (LDCT) screening is now robust and has been formally updated. The National Lung Screening Trial demonstrated that LDCT screening in high-risk smokers reduced lung cancer mortality. The NELSON trial in Europe confirmed and extended these findings.
The American Cancer Society updated its lung cancer screening guideline in November 2023 (published in CA: A Cancer Journal for Clinicians, January–February 2024). The updated criteria represent a significant expansion from the previous 2013 guideline:
The ACS recommends annual low-dose CT screening for asymptomatic individuals aged 50 to 80 years who currently smoke or formerly smoked and have a 20 or greater pack-year smoking history.
Three critical changes from the old guideline:
First, the age range has expanded from 55–74 years to 50–80 years.
Second, the pack-year threshold has been lowered from 30 or more pack-years to 20 or more pack-years.
Third — and this is the most important change — the number of years since quitting smoking is no longer a qualifier for starting or stopping yearly screening. A person who used to smoke with at least a 20 pack-year history, whether they quit yesterday or 20 years ago, is considered to have a high risk for developing lung cancer and should be recommended for a yearly LDCT scan. The ACS has eliminated the years-since-quitting criterion entirely, based on new evidence showing that former smokers' lung cancer risk does not diminish as quickly after cessation as previously assumed.
Note on the USPSTF guideline: The US Preventive Services Task Force still recommends annual LDCT screening for adults aged 50 to 80 with a 20 pack-year history who currently smoke or have quit within the past 15 years. The USPSTF retains the quit-year criterion; the ACS does not. Both agree on the age range of 50–80 and the 20 pack-year threshold.
People should not be screened if serious health problems are likely to significantly limit life expectancy, or if they would be unwilling to undergo evaluation or treatment if cancer is found. Screening involves radiation exposure, the possibility of false positive results, and potential for unnecessary follow-up procedures. The decision to screen should always be made through a shared, informed discussion with a qualified clinician based on individual circumstances.
For the Indian reader: Formal national lung cancer screening guidelines in India are still developing. India currently has nearly 100 million adult smokers, and most patients present with advanced disease (80–85% are incurable), causing nearly 60,000 annual deaths from lung cancer. Indian thoracic oncologists are increasingly recommending that high-risk individuals — those with significant smoking histories, prolonged high-pollution exposure, or other major risk factors — proactively discuss LDCT screening with their pulmonologist. We need to revisit LDCT-based approaches in the Indian context, considering the high burden of air pollution in many heavily populated Indian cities and the increasing incidence of lung cancers among non-smokers in the country.
The Deadly Excuses — Addressed Directly
"I don't smoke. Lung cancer is a smoker's disease."
Between 40 and 50% of lung cancer patients in India are non-smokers, according to multiple Indian clinical studies. Adenocarcinoma — the most common NSCLC subtype — disproportionately affects non-smokers. Air pollution, indoor biomass combustion, secondhand smoke, and genetic factors are all real and clinically established contributors. This belief, if held firmly, is medically dangerous.
"It's just the Delhi pollution. Everyone has a cough."
Air pollution causes respiratory irritation broadly. It is also an established cause of lung cancer. A chronic cough attributable to pollution still deserves evaluation — and the evaluation may reveal something that, caught now, remains treatable.
"I'm too young for lung cancer."
Lung cancer is becoming more common among Indians, particularly among the young and non-smokers, because of the contaminated air they breathe in many areas of the nation. Young-onset NSCLC is increasingly recognised, particularly in non-smokers, and is often associated with specific molecular alterations such as EGFR mutations or ALK rearrangements that carry a better prognosis — if caught in time.
"Tests are too expensive and I may not need them."
The evaluation of a persistent respiratory symptom begins with a consultation and a chest CT scan. The cost of not investigating a symptom that turns out to be early-stage NSCLC is measured not just financially but in the difference between a surgical cure and a lifetime of systemic treatment.
"I'm scared of what they might find."
This is the most human reason of all. Fear of a diagnosis is real and understandable. But the diagnosis does not change based on whether you look for it. What changes is whether you find it at Stage 1, when surgical cure is possible, or at Stage 3 or 4, when the options narrow. The fear itself is not the problem. Letting the fear make your medical decisions for you is.
What You Should Do Right Now
If you or someone close to you has experienced any of the warning signs described in this article — a persistent cough, blood in sputum, unexplained breathlessness, chest pain, hoarseness, unexplained weight loss, or recurring chest infections — here is a clear, immediate plan.
This week: See your general physician or a pulmonologist. Describe all symptoms accurately and completely, including how long they have been present. Do not minimise. Do not say "it's probably nothing" and let the doctor confirm or rule out that assessment through proper evaluation.
Ask specifically about imaging: Depending on your age, symptoms, and risk history, a chest CT scan may be the appropriate first step. Ask your doctor directly whether imaging is indicated for your situation.
Know your risk history before the appointment: Be prepared to discuss your smoking history (including bidis, hookah, and passive exposure), how long you have lived in a high-pollution environment, your occupational exposures, and any family history of lung cancer. This information directly informs the clinical assessment.
If a suspicious lesion is found, ask about biopsy and biomarker testing: Do not allow treatment decisions to be made before comprehensive molecular testing has been completed. Ask specifically about EGFR mutation testing, ALK and ROS1 rearrangement testing, PD-L1 expression, and other actionable biomarkers. The results will determine which treatments are most appropriate — and may identify eligibility for targeted oral therapies that are significantly more effective than chemotherapy for certain mutations.
Consider a second opinion for complex cases: Lung cancer management is one of the most rapidly evolving fields in oncology. If you are uncertain about a diagnosis, staging, or treatment recommendation, a second opinion from a thoracic oncology specialist at a high-volume cancer centre is not a sign of distrust — it is standard practice and is actively encouraged by leading oncology organisations.
Professional Support Options
If you are experiencing possible lung cancer symptoms, seeking a second opinion on a diagnosis, or unsure which diagnostic tests or treatment options are right for your individual situation, do not wait. Speak with a qualified oncologist today.
Connect with experienced U.S.-based cancer specialists for a comprehensive second-opinion consultation. They will carefully review your case and help determine the most appropriate next steps for your individual health needs:
👉 https://myamericandoctor.com/our-doctors/
You may also choose to enrol in our upcoming concierge medical clinic in India, Global Concierge Doctors. We offer U.S.-style primary care with 24/7 access to India-based physicians for ongoing guidance on any health concern. When required, we coordinate referrals to trusted specialists in India and the U.S. for advanced evaluation and care.
Your health decisions today shape your life tomorrow.
The Final Word
NSCLC does not announce itself loudly. It arrives as a cough you blame on the weather, a breathlessness you attribute to ageing, a fatigue you explain away with a busy schedule. By the time it makes itself undeniable, it has often already used the time you gave it.
And yet: oncology in 2025 has more tools than it has ever had. Targeted therapies have given years of quality life to patients with actionable mutations. Immunotherapy has produced durable responses in cancers once considered rapidly fatal. Surgery at Stage 1 offers the genuine possibility of cure. The updated ACS screening guideline means that millions more people — including former smokers who quit years ago — are now formally eligible for early detection through annual low-dose CT.
What those tools require is time — specifically, the time you give your oncologist to find this disease while it is still localised, still treatable, still something that medicine can address decisively.
You have read this far. Something may have prompted you to look this up. A cough. A worry. A family member you are concerned about.
That instinct is worth following. Book the appointment. Not next month. This week. Your lungs have been asking for your attention. Now is the time to listen.
Reader Poll
Have you or someone you know experienced persistent respiratory symptoms and delayed seeking medical evaluation?
- [ ] Yes, and I am booking an appointment this week
- [ ] Yes, I have been putting it off
- [ ] No, I sought evaluation promptly
- [ ] No relevant symptoms currently
Share This Article
Know someone who has been dismissing a cough that has stayed too long? A long-term bidi smoker who has not had a chest evaluation? A non-smoker in a heavily polluted city who assumes they are not at risk? Share this article. It may be the prompt that matters.
Last Updated: 18th February 2026
Medical Disclaimer
This article is provided strictly for educational, informational, and awareness purposes only. The real-life patient stories and examples shared in this article are drawn from clinical experiences, patient interactions, and commonly observed scenarios in oncology practice. They are presented for educational and awareness purposes only. Names and identifying details have been changed to protect patient privacy. While these accounts reflect authentic experiences encountered in medical practice, they have not been independently documented or published by us as formal case studies. Individual experiences with cancer diagnosis, treatment, and outcomes vary widely, and no single story should be taken as representative of what any reader may experience. It is not intended to be, and should not be construed as, professional medical advice, diagnosis, treatment, or a substitute for consultation with qualified healthcare professionals.
No Doctor-Patient Relationship
The information presented in this article does not establish a doctor-patient relationship between the reader and the author, publisher, or any affiliated entities. No medical decisions should be made based solely on the content of this article.
Consult Qualified Medical Professionals
If you are experiencing any symptoms mentioned in this article, have been diagnosed with cancer, or have concerns about cancer risk, seek immediate consultation with qualified oncologists, physicians, or appropriate medical specialists. For medical emergencies, contact emergency services immediately.
Individual Medical Situations Vary
Every person's medical condition, health history, risk factors, cancer type, and circumstances are unique. Diagnostic tests, treatment options, and medical recommendations must be tailored to individual patients through direct consultation with licensed healthcare providers who have access to complete medical histories and can perform proper clinical evaluations.
Not a Recommendation for Specific Tests or Treatments
References to biopsies, imaging studies (CT scans, PET scans, MRI), blood tests, tumour markers, chemotherapy, radiation therapy, immunotherapy, targeted therapy, surgery, or any other diagnostic procedures and treatments in this article are for informational purposes only and do not constitute recommendations that you should or should not undergo these tests or treatments. All decisions regarding medical testing, diagnosis, and treatment should be made in consultation with qualified healthcare professionals based on your specific medical situation.
No Guarantee of Accuracy or Completeness
While efforts have been made to provide accurate information, medical knowledge continuously evolves, particularly in the rapidly advancing field of oncology. The information in this article may not reflect the most current research, clinical guidelines, treatment protocols, or medical practices. The author and publisher make no representations or warranties regarding the accuracy, completeness, or timeliness of the content.
Do Not Disregard or Delay Professional Medical Advice
Never disregard, avoid, or delay obtaining professional medical advice from qualified healthcare providers because of something you have read in this article. If you have questions or concerns about information presented here, discuss them with your personal physician or oncologist. Early detection and prompt treatment significantly improve cancer outcomes.
Third-Party Resources and Links
Any references to third-party medical services, clinics, doctors, cancer centres, or external websites are provided for informational purposes only and do not constitute endorsements. The author and publisher are not responsible for the content, services, or practices of any third-party entities.
Limitation of Liability
To the fullest extent permitted by law, the author, publisher, and affiliated entities disclaim all liability for any direct, indirect, incidental, consequential, or punitive damages arising from the use of, or reliance on, information contained in this article. This includes, but is not limited to, medical complications, treatment decisions, financial losses, or any other adverse outcomes.
Geographic and Regulatory Considerations
Medical regulations, standards of care, insurance coverage, availability of diagnostic tests, treatment protocols, and access to cancer therapies vary by country, region, and healthcare system. Information regarding costs, procedures, and medical practices may not be applicable to all geographic locations or healthcare settings.
Clinical Trials and Experimental Treatments
Any references to clinical trials, experimental treatments, or investigational therapies are for informational purposes only. Participation in clinical trials should only be considered after thorough discussion with your oncology team and a full understanding of all risks and benefits.
Your Responsibility
You acknowledge that you are solely responsible for your own health decisions and that you will consult with appropriate licensed healthcare professionals before making any medical decisions or undergoing any diagnostic tests or treatments.
Acknowledgment
By reading and using the information in this article, you acknowledge that you have read, understood, and agreed to this disclaimer in its entirety. You further acknowledge that this article has been created with the assistance of artificial intelligence. While every effort has been made to ensure accuracy, AI-generated content may occasionally contain errors, omissions, or inaccuracies. The information presented here is intended solely for educational and informational purposes and should not be relied upon as a substitute for professional medical advice. Readers are strongly encouraged to consult qualified healthcare professionals, refer to peer-reviewed medical literature, and cross-reference information from established clinical sources before making any health-related decisions.
Sources Consulted for This Article
This article has been written with reference to the following authoritative sources, verified through live web browsing during preparation:
American Cancer Society — Screening for Lung Cancer: 2023 Guideline Update (CA: A Cancer Journal for Clinicians, November 2023 / January–February 2024); ACS Cancer Facts & Figures 2025; ACS Non-Small Cell Lung Cancer Treatment Pages (last revised June 2025) | ASCO Living Guidelines — Therapy for Stage IV NSCLC With Driver Alterations, Version 2025.1; Therapy for Stage IV NSCLC Without Driver Alterations, Version 2025.1; Management of Stage III NSCLC: ASCO Guideline Rapid Recommendation Update (2024) | NCI PDQ — Non-Small Cell Lung Cancer Treatment (Health Professional Version), May 2025 | NCCN Guidelines — Non-Small Cell Lung Cancer, Version 4.2025 | PMC/PubMed — Update 2025: Management of Non-Small Cell Lung Cancer (PMC11937135); Advances in NSCLC: Current Insights and Future Directions (PMC11278207); Evaluation of Risk Factors for Lung Cancer Among Never Smokers (AIIMS Bhubaneswar, Cureus 2024, PMC10991854); Lung Cancer Screening in India (Indian Journal of Medical Research, PMC11801781) | The Lancet Regional Health — Southeast Asia — Uniqueness of Lung Cancer in Southeast Asia (July 2024) | JCO Global Oncology — Association of Tobacco Use and Cancer Incidence in India (2024) | South India 15-year cross-sectional histopathology study (PMC12173675)
What's Your Reaction?
 Like
0
Like
0
 Dislike
0
Dislike
0
 Love
0
Love
0
 Funny
0
Funny
0
 Angry
0
Angry
0
 Sad
0
Sad
0
 Wow
0
Wow
0