Your Immune System Is Fighting Cancer Right Now (And Losing. Here's Why.)
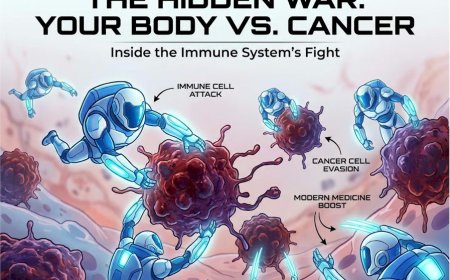
Your immune system destroys abnormal cells every day, preventing cancer before it starts. But cancer cells evolve sophisticated strategies to hide from, disable, and even weaponize your immune defenses. This creates a silent battle inside your body where your natural protection fails despite being perfectly healthy. Understanding tumor immunology—how cancer escapes immune detection through checkpoint proteins, suppressor cells, and camouflage techniques—explains why "boosting immunity" doesn't prevent cancer, why immunotherapy revolutionizes treatment, and most critically, why you cannot rely on your immune system alone. Early screening catches what your immunity misses. Your life depends on this knowledge.
AT A GLANCE
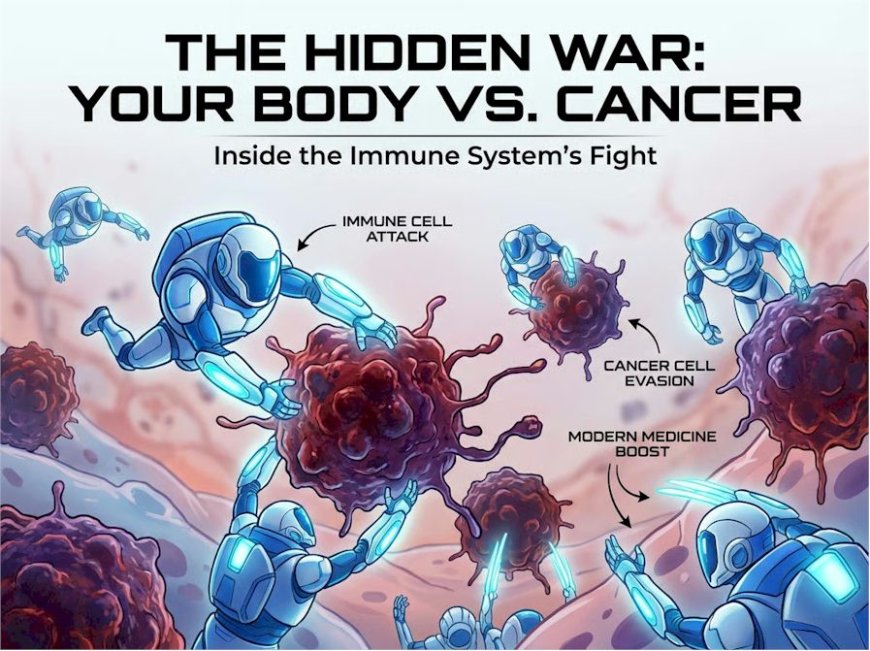
Your body is designed to kill cancer cells. Every single day, your immune system hunts down and destroys abnormal cells before they become tumors. It's happening right now as you read this sentence. But here's what terrifies oncologists: cancer has learned to hide from your immune system, to trick it, to shut it down completely. Understanding how your immune system fights cancer — and why it sometimes fails — could be the difference between catching cancer early and facing a diagnosis when it's too late. This article reveals the hidden war happening inside your body, why your natural defenses aren't always enough, and what modern medicine is doing to turn your immune system into cancer's worst nightmare.
The War You Don't Know You're Fighting
Right now.
This very second.
Inside your body, there's a battle raging.
Your immune system — the same defense network that fights off the flu, heals cuts, and destroys bacteria — is hunting cancer cells.
Not might be. Not could be. IS.
Because here's what most people don't know: your body creates abnormal cells every single day. Cells that don't follow normal growth rules. Cells that could become cancer.
And most of the time, your immune system finds them. Destroys them. You never even know it happened.
You wake up. Have your coffee. Go to work. Completely unaware that your T-cells just eliminated a cluster of pre-cancerous cells in your colon.
But sometimes — and this is the terrifying part — cancer wins.
Not because your immune system is weak. Not because you did something wrong.
But because cancer cells are INCREDIBLY good at hiding, at disguising themselves, at turning your own defense system against you.
Sound like science fiction?
It's happening in millions of people right now. Maybe even in you.
Here's The Brutal Truth About Your Immune System and Cancer
Let me be very direct about something your doctor may not always have time to explain fully:
Your immune system SHOULD kill cancer before it becomes a problem.
That's its job. That's what it's designed to do.
So when someone gets diagnosed with cancer, the real question isn't "Why did I get cancer?"
The real question is: "Why did my immune system FAIL to stop it?"
And the answer changes everything about how we understand and treat cancer.
The Two Possibilities You're Facing
Option 1: Your Immune System Is Working
Your T-cells are patrolling. Finding abnormal cells. Killing them before they become tumors. You'll never get cancer from these cells because your natural defenses are doing their job perfectly.
You don't need to do anything. This is happening automatically, right now.
Option 2: Cancer Has Found a Way to Hide
Cancer cells have developed "immune escape mechanisms." They've learned to disguise themselves as normal cells, turn off your immune system's attack signals, create an environment where immune cells can't function, and actually RECRUIT your immune system to help the tumor grow.
And when this happens, your body's natural defenses become useless. Cancer grows unchecked while your immune system stands by, completely blind to the threat.
This is why immunotherapy — treatments that help your immune system "see" cancer again — has revolutionised oncology in the past decade.
The Silent Betrayal Inside Your Body
Let me walk you through what's happening inside you right this moment:
Week 1–2: When Your Immune System Works Perfectly
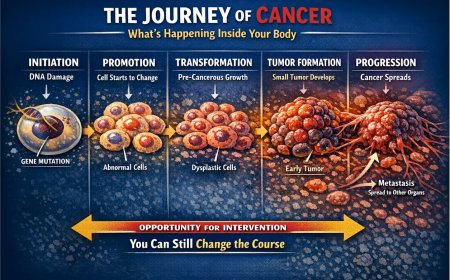
A cell in your body mutates. Maybe from sun damage. Maybe from a virus. Maybe from random chance during cell division.
This abnormal cell displays unusual proteins on its surface — like a criminal wearing the wrong uniform.
Your immune system's scout cells (dendritic cells) notice immediately. They grab these unusual proteins and rush to your lymph nodes.
"Alert! We've got an abnormal cell in Sector 7-B!"
Your T-cells mobilise. They learn to recognise this specific abnormal protein. They multiply into an army.
They travel to the site. Find the abnormal cell. Destroy it completely.
Result: You never knew anything happened. Cancer prevented before it started.
This is your immune system working as designed.
Month 1–3: When Cancer Starts to Hide
But now imagine a different scenario. That abnormal cell mutates again. And again.
By random chance, one mutation does something clever: it reduces the display of those unusual proteins on its surface.
Your immune system's scouts pass right by it. "Nothing to see here. Looks normal to us."
The cancer cell divides. Two becomes four. Four becomes eight.
Some daughter cells have even better camouflage. Some develop proteins that actively SUPPRESS immune responses.
Your immune system is right there. Immune cells are surrounding the emerging tumour. But they can't "see" the cancer cells anymore.
Like a burglar who's learned the security system's blind spots.
Month 4–12: When Cancer Weaponises Your Immune System
This is where it gets truly sinister.
Advanced tumours don't just hide from your immune system. They turn it into an ally.
The tumour secretes chemicals that attract regulatory T-cells — the immune cells whose job is to PREVENT inflammation and immune responses.
Why? Because uncontrolled inflammation damages normal tissue. Your body needs these regulatory cells to prevent autoimmune diseases.
But cancer hijacks this safety mechanism.
The tumour becomes surrounded by regulatory T-cells that actively SUPPRESS the killer T-cells trying to attack the cancer.
Your immune system is now protecting the tumour. Your own defence mechanism has been reprogrammed to help cancer grow.
The tumour has created an "immune-privileged sanctuary" — a zone where immune attack is switched off.
And all of this happens without a single symptom.
You feel fine. You're going about your daily life. While inside, cancer is building an empire protected by your own immune system.
Real Stories That Should Wake You Up
Story #1: Amit, 42, Mumbai
Amit was healthy. Ran marathons. Never smoked. Ate well. "I'm the last person who'd get cancer," he told his wife.
He noticed a persistent cough. "Probably pollution. Mumbai air, you know."
He waited six months. Finally saw a doctor when he started coughing blood.
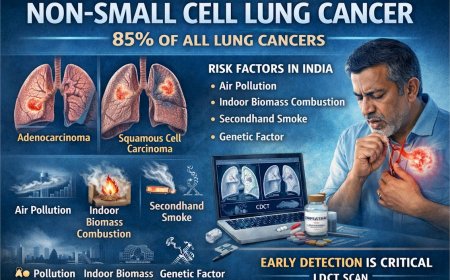
Non-small cell lung cancer. Stage 3B. Never smoked a day in his life.
"How?" he asked the oncologist. "I thought my immune system would catch something like this."
"Your immune system DID try to catch it," the doctor explained. "We can see evidence of immune response in your biopsy. But the tumour developed PD-L1 proteins — essentially an 'off switch' for your T-cells. Your immune system was right there, surrounding the tumour, but it couldn't attack."
Amit received chemotherapy plus immunotherapy (pembrolizumab). The immunotherapy blocked those PD-L1 proteins, re-enabling his immune system to attack the cancer. His tumour shrunk significantly in three months. Not cured — but the cancer that his immune system couldn't see suddenly became visible again.
His words: "I had no idea my own body had an army that just needed the right orders. The immunotherapy didn't kill the cancer — it let MY immune system finally do its job."
Please note: this story is illustrative. Individual outcomes with immunotherapy vary considerably depending on cancer type, stage, biomarker profile, and overall health.
The Five Deadly Misconceptions About Immunity and Cancer
Misconception #1: "If I have a strong immune system, I won't get cancer"
Cancer doesn't develop because your immune system is "weak." It develops because cancer cells EVOLVE to escape immune detection.
Even elite athletes with incredibly robust immune systems get cancer. Why? Because immune strength against infections doesn't equal immune detection of cancer.
Cancer cells are YOUR cells. They're just mutated. They don't carry foreign proteins the way viruses or bacteria do. Your immune system has to recognise very subtle differences between cancer cells and normal cells. It's like trying to spot a spy who looks almost exactly like a citizen.
A "strong" immune system that fights off colds easily might still completely miss cancer cells that have learned perfect camouflage.
Misconception #2: "Cancer only happens when your immune system is compromised"
Yes, immunocompromised people have higher cancer rates. But most cancer patients have perfectly normal immune systems.
The issue isn't that your immune system is too weak. The issue is that cancer has learned to hide from a normal, functioning immune system.
Immunosuppressed patients do get certain cancers more frequently — particularly virus-related cancers and some lymphomas. But the majority of common cancers (breast, lung, colon, prostate) occur in people with completely normal immune function.
Your immune system isn't failing because it's weak. It's being outsmarted.
Misconception #3: "Boosting my immune system will prevent cancer"
There is no credible scientific evidence that general "immune-boosting" supplements prevent cancer.
Why? Because the problem isn't that your immune system is underactive. The problem is that cancer has developed specific escape mechanisms.
What you need isn't a "stronger" immune system. You need an immune system that can recognise cancer's disguises, overcome cancer's suppressive signals, and penetrate the tumour's protective environment.
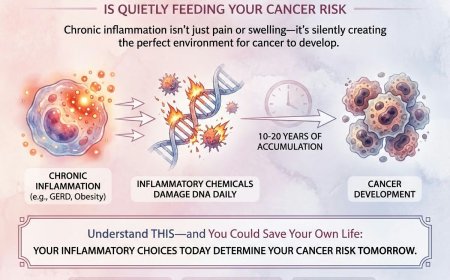
Random immune stimulation doesn't accomplish this. In fact, excessive immune activation can cause chronic inflammation that may actually PROMOTE cancer growth in certain contexts.
Misconception #4: "If my immune system didn't catch it early, it's hopeless"
Even advanced cancers are surrounded by immune cells. Your immune system hasn't given up. It's just been temporarily disabled.
Modern immunotherapy can reactivate it. We now have treatments that block cancer's "invisibility cloak" (checkpoint inhibitors), train your immune system to recognise cancer (cancer vaccines), and engineer your own T-cells to hunt specific cancer markers (CAR-T therapy).
Your immune system is still there. Still capable. It just needs help seeing the target.
Misconception #5: "Immunotherapy is the miracle cure for all cancers"
Immunotherapy is revolutionary. But it doesn't work for everyone or every cancer type.
Current response rates vary widely. Some melanoma patients experience dramatic, long-lasting responses. Some lung cancer patients see significant tumour shrinkage. Many other cancer types show limited or no response.
Immunotherapy works best when the cancer has certain biomarkers (such as PD-L1 expression or high tumour mutation burden), when the patient's immune system remains functional, and when the tumour hasn't created an extremely suppressive microenvironment.
It's not a magic bullet. But for patients who respond, it can be life-changing.
The key — always — is early detection, so you have the widest possible range of treatment options available.
What's Really Happening: The Science Your Doctor Might Not Always Have Time to Explain
Your Immune System's Cancer-Fighting Team
The Scouts: Dendritic Cells
These are your immune system's intelligence agents. They patrol your body, sampling proteins from every cell they encounter. When they find unusual proteins, they rush to lymph nodes and present them to T-cells: "Here's what the enemy looks like. Memorise this."
The Assassins: Cytotoxic T-Cells (CD8+ T-cells)
Once trained to recognise cancer markers, these cells multiply and hunt. When they find a cell displaying the target protein, they inject toxins that cause the cancer cell to self-destruct.
The Generals: Helper T-Cells (CD4+ T-cells)
These coordinate the immune response, calling in reinforcements and organising the attack strategy.
The Patrol Officers: Natural Killer Cells
These patrol your body looking for cells that have lost their normal identification markers. Cancer cells often reduce these markers to hide from T-cells — but that loss of identity actually makes them visible to NK cells instead.
Cancer's Counter-Strategies
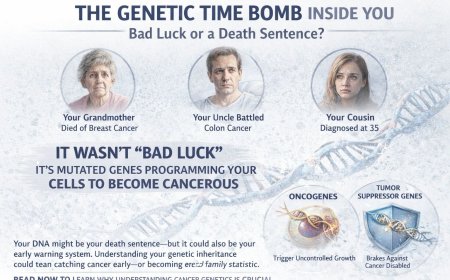
Strategy #1: Reduce Surface Markers (Invisibility)
Cancer cells reduce MHC-I molecules — the "ID badges" that display cell proteins to T-cells. Without proper ID display, T-cells can't identify cancer cells as abnormal.
Strategy #2: Express Checkpoint Proteins (Off Switch)
Cancer cells display PD-L1 or other "checkpoint" proteins that tell T-cells: "Stand down. I'm normal. Don't attack." It's like showing a fake police badge. T-cells receive the signal and abort their attack.
Strategy #3: Recruit Suppressor Cells (Bodyguards)
Tumours secrete chemicals that attract regulatory T-cells and myeloid-derived suppressor cells — immune cells that PREVENT immune responses. These cells surround the tumour, creating a protective shield.
Strategy #4: Create a Hostile Environment (Fortress)
Tumours create areas of low oxygen, high acidity, and metabolic disruption — conditions where T-cells can't function properly. Even if T-cells reach the tumour, they can be disabled by the hostile microenvironment.
How Modern Immunotherapy Fights Back
Checkpoint Inhibitors (Removing the Off Switch)
Drugs like pembrolizumab, nivolumab, and atezolizumab block checkpoint proteins. When cancer can't activate the "off switch," T-cells can attack normally.
CAR-T Therapy (Engineering Super Soldiers)
Doctors extract your T-cells, genetically engineer them to recognise specific cancer markers, multiply them to millions, and infuse them back into you. These engineered cells hunt cancer with precision.
Cancer Vaccines (Training the Army)
These are therapeutic vaccines — distinct from preventive vaccines like the HPV vaccine. They train your immune system to recognise and attack specific cancer proteins already present in the body.
Cytokine Therapy (Calling in Reinforcements)
Therapies such as IL-2 and IFN-alpha can amplify immune responses, though they carry significant side effect profiles and have largely been superseded by newer immunotherapy approaches in many cancer types.
What You MUST Do Right Now
Understand Your Risk
Know Your Family History. Which relatives had cancer? What types? At what ages? Family history can indicate whether you carry genetic vulnerabilities in immune surveillance pathways.
Identify Your Risk Factors. Smoking and tobacco use can suppress immune function and directly damage DNA. Chronic viral infections — particularly HPV, Hepatitis B and C, and HIV — impair immune surveillance. Immunosuppressive medications and chronic inflammatory conditions also affect the immune system's ability to monitor for abnormal cells.
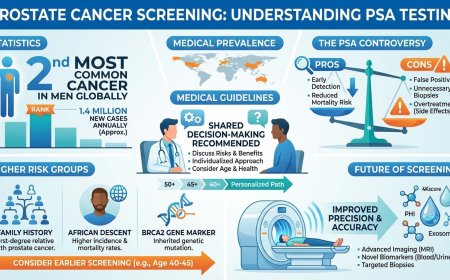
Schedule Age-Appropriate Screening — Based on Current Guidelines
Your immune system may be working perfectly. But screening provides the backup it sometimes needs.
The following guidelines are drawn from current recommendations by the American Cancer Society (ACS), the U.S. Preventive Services Task Force (USPSTF), and related bodies as of early 2026. Because guidelines can change, always confirm the most appropriate schedule with your own physician.
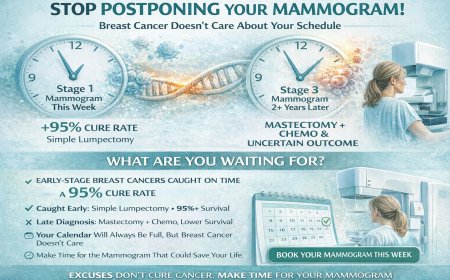
Breast Cancer Screening
The ACS recommends that women aged 40 to 44 have the option to begin annual mammography screening if they wish to do so. Women aged 45 to 54 should get mammograms every year. Women 55 and older may switch to mammograms every two years, or continue yearly screening. Screening should continue as long as a woman is in good health and expected to live at least 10 more years. High-risk women — those with BRCA gene mutations, a strong family history, or a history of chest radiation before age 30 — should discuss earlier and more frequent screening (often beginning at age 30 with both MRI and mammogram) with their doctor. Note: The ACS does not currently recommend routine clinical breast self-exams as a formal screening method, as evidence for their benefit in conjunction with regular mammography is limited. However, all women should be familiar with how their breasts normally look and feel, and report any changes to a doctor promptly.
Colorectal Cancer Screening
Adults at average risk should begin colorectal cancer screening at age 45. A colonoscopy every 10 years is one accepted option; other stool-based and visual tests are also available and should be discussed with your physician. Screening continues through age 75 for average-risk adults. Between ages 76 and 85, screening decisions should be made jointly with your doctor based on your personal health and history.
Lung Cancer Screening
The ACS recommends annual low-dose CT (LDCT) screening for adults aged 50 to 80 who have at least a 20-pack-year smoking history and currently smoke or have formerly smoked. Importantly, unlike older guidelines, there is no longer a cut-off based on years since quitting — research now confirms that lung cancer risk remains elevated well beyond 15 years after cessation. Before beginning screening, a shared discussion with a healthcare professional is recommended to understand benefits, limits, and potential harms.
Cervical Cancer Screening
Women and individuals with a cervix at average risk should begin cervical cancer screening at age 25. Primary HPV testing every five years (clinician-collected) is the preferred approach. A self-collected vaginal HPV test every three years is now also an accepted option following updated ACS guidelines released in December 2025. A co-test (HPV plus Pap) every five years, or a Pap smear alone every three years if HPV testing is unavailable, are also acceptable. Screening continues until at least age 65, provided recent tests have been normal. You should be screened even if you have received the HPV vaccine.
Skin Cancer Awareness
People with significant sun exposure history or a family history of melanoma should discuss skin examination with their doctor. There is no universal consensus guideline recommending routine screening skin exams for the general population, but awareness of changes to existing moles and new skin lesions remains important.
Don't Trust Your Immune System Alone
If you have ANY of the following, see a doctor promptly — do not wait:
An unexplained lump anywhere in the body. A persistent cough lasting more than three weeks. Unexplained weight loss of more than 4–5 kg over three months. Changes in bowel or bladder habits that are new or persistent. Unusual bleeding or discharge. Skin changes or a mole that is changing in size, shape, or colour. Persistent fatigue not relieved by rest.
Your immune system might be fighting cancer right now — and losing. These symptoms require evaluation. Don't wait for your immune system to win on its own.
Get checked.
Professional Support Options
If you're experiencing possible cancer symptoms, seeking a second opinion, or unsure which tests or treatments are right for you, don't wait. Speak with a qualified oncologist today.
Connect with experienced U.S.-based cancer specialists for a comprehensive second-opinion consultation. They will carefully review your case and help determine the most appropriate next steps for your individual health needs:
👉 https://myamericandoctor.com/our-doctors/
You may also choose to enrol in the upcoming concierge medical clinic in India, Global Concierge Doctors. This service offers U.S.-style primary care with 24/7 access to India-based physicians for ongoing guidance on any health concern. When required, referrals are coordinated to trusted specialists in India and the U.S. for advanced evaluation and care.
Your health decisions today shape your life tomorrow.
The Final Word: What Your Immune System Can't Tell You
If your immune system could speak, here's what it would say:
"I'm fighting for you every single day. I've destroyed thousands of abnormal cells you never knew existed."
"But I'm not perfect. Cancer is smart. It evolves. It hides. It cheats."
"I need backup. I need screening tests to catch what I miss. I need early detection to give me a fighting chance."
"And if cancer outsmarts me, I need modern medicine — immunotherapy, surgery, radiation — to help me finish the fight."
"I'm your first line of defence. But I can't be your only line of defence."
"Help me help you. Get screened. Pay attention to symptoms. Don't wait."
Take Action NOW
Step 1: Acknowledge that your immune system, while extraordinary, can be outsmarted by cancer.
Step 2: Schedule your age-appropriate cancer screening this week.
Step 3: If you have concerning symptoms, book a doctor's appointment today.
Step 4: Learn your family cancer history and discuss it with your doctor.
Step 5: Stop trusting "immune-boosting" supplements and start trusting evidence-based screening.
Your immune system is fighting for you right now. But it needs help.
Give it that help. Today.
Reader Poll
Do you rely on your immune system to prevent cancer?
[ ] Yes, and now I'm scheduling screening tests [ ] Yes, and I'm now concerned about my approach [ ] No, I already get regular screening [ ] I didn't know cancer could escape immune detection
Share This Article
Know someone who believes a "strong immune system" is enough to prevent cancer? Know someone who's avoiding screening because they "feel healthy"?
Share this article. It might help them understand why screening matters even when you feel fine.
Medical Disclaimer
This article is provided strictly for educational, informational, and awareness purposes only. It is not intended to be, and should not be construed as, professional medical advice, diagnosis, treatment, or a substitute for consultation with qualified healthcare professionals.
No Doctor-Patient Relationship
The information presented in this article does not establish a doctor-patient relationship between the reader and the author, publisher, or any affiliated entities. No medical decisions should be made based solely on the content of this article.
Consult Qualified Medical Professionals
If you are experiencing any symptoms mentioned in this article, have been diagnosed with cancer, or have concerns about cancer risk, seek immediate consultation with qualified oncologists, physicians, or appropriate medical specialists. For medical emergencies, contact emergency services immediately.
Individual Medical Situations Vary
Every person's medical condition, health history, risk factors, cancer type, and circumstances are unique. Diagnostic tests, treatment options, and medical recommendations must be tailored to individual patients through direct consultation with licensed healthcare providers who have access to complete medical histories and can perform proper clinical evaluations.
Not a Recommendation for Specific Tests or Treatments
References to biopsies, imaging studies (CT scans, PET scans, MRI), blood tests, tumour markers, chemotherapy, radiation therapy, immunotherapy, targeted therapy, surgery, or any other diagnostic procedures and treatments in this article are for informational purposes only and do not constitute recommendations that you should or should not undergo these tests or treatments. All decisions regarding medical testing, diagnosis, and treatment should be made in consultation with qualified healthcare professionals based on your specific medical situation.
No Guarantee of Accuracy or Completeness
While efforts have been made to provide accurate information, medical knowledge continuously evolves, particularly in the rapidly advancing field of oncology. The information in this article may not reflect the most current research, clinical guidelines, treatment protocols, or medical practices. The author and publisher make no representations or warranties regarding the accuracy, completeness, or timeliness of the content.
Do Not Disregard or Delay Professional Medical Advice
Never disregard, avoid, or delay obtaining professional medical advice from qualified healthcare providers because of something you have read in this article. If you have questions or concerns about information presented here, discuss them with your personal physician or oncologist. Early detection and prompt medical attention significantly improve cancer outcomes.
Third-Party Resources and Links
Any references to third-party medical services, clinics, doctors, cancer centres, or external websites are provided for informational purposes only and do not constitute endorsements. The author and publisher are not responsible for the content, services, or practices of any third-party entities.
Limitation of Liability
To the fullest extent permitted by law, the author, publisher, and affiliated entities disclaim all liability for any direct, indirect, incidental, consequential, or punitive damages arising from the use of, or reliance on, information contained in this article. This includes, but is not limited to, medical complications, treatment decisions, financial losses, or any other adverse outcomes.
Geographic and Regulatory Considerations
Medical regulations, standards of care, availability of diagnostic tests, treatment protocols, and access to cancer therapies vary by country, region, and healthcare system. Information regarding procedures and medical practices may not be applicable to all geographic locations or healthcare settings.
Clinical Trials and Experimental Treatments
Any references to clinical trials, experimental treatments, or investigational therapies are for informational purposes only. Participation in clinical trials should only be considered after thorough discussion with your oncology team and a full understanding of all risks and benefits.
Your Responsibility
You acknowledge that you are solely responsible for your own health decisions and that you will consult with appropriate licensed healthcare professionals before making any medical decisions or undergoing any diagnostic tests or treatments.
Acknowledgment
By reading and using the information in this article, you acknowledge that you have read, understood, and agreed to this disclaimer in its entirety. You further acknowledge that this article has been created with the assistance of artificial intelligence. While every effort has been made to ensure accuracy, AI-generated content may occasionally contain errors, omissions, or inaccuracies. The information presented here is intended solely for educational and informational purposes and should not be relied upon as a substitute for professional medical advice. Readers are strongly encouraged to consult qualified healthcare professionals, refer to peer-reviewed medical literature, and cross-reference information from established clinical sources before making any health-related decisions.
Last Updated: 5th February 2026
What's Your Reaction?
 Like
0
Like
0
 Dislike
0
Dislike
0
 Love
0
Love
0
 Funny
0
Funny
0
 Angry
0
Angry
0
 Sad
0
Sad
0
 Wow
0
Wow
0