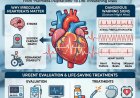
Your Cardiologist Says "Everything is Normal" — But Your Chest Pain Continues. What Should You Do Now?
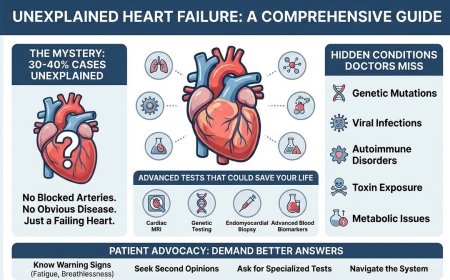
Persistent chest discomfort, unexplained fatigue, or shortness of breath—despite “normal” heart tests—can leave patients confused and unheard. This guide empowers individuals to take control of their heart health with a clear, step-by-step action plan. Learn how to document symptoms effectively, organize medical records, seek the right second opinion, and ask informed questions about advanced cardiac imaging such as cardiac MRI. Designed for patients navigating uncertainty, this article emphasizes self-advocacy, timely evaluation, and informed decision-making—helping you move from vague reassurances to clear, confident answers about your heart.

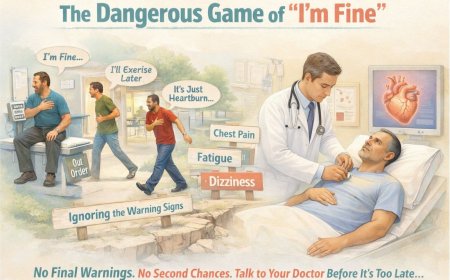
You’re sitting in your cardiologist’s office, clutching the armrest a little too tightly. You’ve just described what’s been happening—the chest discomfort, the unexplained fatigue, the shortness of breath that shouldn’t be happening.
Your doctor reviews your ECG. Checks your stress test results. Glances at your echo report.
“Everything looks normal. Try to relax. Come back in six months.”
But you know something isn’t right. Your body is telling you a story that your test results aren’t confirming.
So what do you do now?
If this sounds familiar, you’re not alone. Many patients experience persistent cardiac-type symptoms while standard testing looks reassuring or inconclusive. The goal isn’t to panic—or to ignore it. The goal is to escalate thoughtfully, document clearly, and push for the right next step when symptoms and test results don’t align.
Below is a practical action plan you can use to advocate for yourself and help your clinician see what you’re experiencing with maximum clarity.
Step 1: Document Your Symptoms Like a Medical Detective
Why this matters
A cardiologist may see dozens of patients each week. Broad statements like “I get chest pain sometimes” or “I’m tired a lot” are easy to underestimate—especially when baseline tests look normal. Specific patterns, triggers, and timelines are harder to dismiss and often reveal what the next diagnostic step should be.
Create your symptom diary (start today)
For the next 2 weeks (or until your next appointment), track every episode.
What to record each time:
-
Date + exact time (use a phone timestamp)
-
Location (center of chest? left side? upper abdomen? back?)
-
Type of sensation (pressure, tightness, burning, sharp, heaviness)
-
Duration (seconds vs minutes vs longer)
-
Intensity (1–10)
-
What you were doing (stairs, walking, resting, after meals, emotional stress, cold exposure)
-
What relieved it (rest, posture change, antacids, inhaler, nitroglycerin—if prescribed)
-
Associated symptoms (shortness of breath, sweating, nausea, dizziness, palpitations, faintness)
-
Anything unusual that day (poor sleep, dehydration, heavy caffeine, infection/fever)
Example: vague vs specific
❌ Vague: “I get chest pain sometimes, especially when I’m stressed.”
✅ Specific: “Over the past 3 weeks, I’ve had 7 episodes of pressure-like discomfort in the center of my chest. Each lasted 5–8 minutes. Five occurred while climbing stairs to my 3rd-floor apartment, one after a heavy meal, one during an argument. Intensity was ~6/10. It did not radiate. It resolved within 2 minutes of sitting down. No sweating or nausea, but mild shortness of breath during episodes.”
That second description doesn’t sound like “background noise.” It sounds like clinical data.
Use technology to make it easier
-
Notes app: one dedicated “Heart Symptoms” note
-
Voice memo: record immediately after an episode
-
Wearables: capture heart rate trends (helpful, not definitive)
-
Photos: swelling, color change, visible signs (if present)
Your diary becomes objective evidence—and it often helps you and your doctor spot patterns you wouldn’t notice in hindsight.
Step 2: Organize Your Complete Medical History (So Nothing Gets Missed)
Walk into your visit with a clear one-document summary. This saves time and prevents important details from getting lost.
A. Tests you’ve already had
List each test with date + the key details from the report.
ECG (Electrocardiogram):
-
Date performed
-
Report language (e.g., “normal sinus rhythm,” “nonspecific ST-T changes”)
-
Where it was done
Stress test:
-
Date performed
-
Type (exercise treadmill vs pharmacologic)
-
How long you exercised / stage achieved
-
Whether target heart rate was reached (approx. percent of age-predicted max)
-
Result: negative / positive / equivocal / inconclusive
Echocardiogram:
-
Date performed
-
Ejection fraction if mentioned
-
Valve findings (regurgitation/stenosis/prolapse)
-
Any wall motion abnormalities
-
Any comment about pulmonary pressures
Blood work (if done recently):
-
Lipid panel (Total, LDL, HDL, triglycerides)
-
HbA1c / fasting glucose
-
Troponin (if checked during symptoms)
-
BNP/NT-proBNP (if shortness of breath/heart failure concern)
-
Thyroid and anemia testing if fatigue is prominent (common “look-alikes”)
Other imaging / workups:
-
Chest X-ray / CT chest
-
Coronary CT angiography (if done)
-
Cardiac MRI (if done)
-
Prior angiogram (if done)
B. Current medications and supplements
Include exact doses and timing:
-
Heart and BP meds
-
Diabetes meds
-
Cholesterol meds
-
OTC meds (especially NSAIDs, decongestants, stimulant weight-loss products)
-
Supplements/herbals (some affect BP, rhythm, bleeding risk)
Also note: what changed recently and any side effects.
C. Family history (this often changes the entire strategy)
Document:
-
Heart attacks or bypass/stents: who + age at diagnosis
-
Sudden unexplained death: who + age + circumstances
-
Known genetic conditions (HCM, long QT, arrhythmogenic cardiomyopathy, familial hypercholesterolemia, Marfan, etc.)
-
Stroke, diabetes, hypertension in first-degree relatives
D. Your risk factors (honesty helps your plan)
-
Smoking history (including past)
-
Diabetes / pre-diabetes
-
Hypertension
-
Cholesterol issues
-
Weight and activity level
-
Sleep quality (snoring, apnea, daytime sleepiness)
-
Alcohol and stimulants
-
Stress and anxiety (important—but not automatically “the cause”)
Why this matters
It does three powerful things:
-
Saves consultation time for next steps
-
Signals you’re a serious, engaged patient
-
Reveals patterns across tests that are easy to miss when each result is viewed alone
If possible, send this document to the clinic before your visit.
Step 3: Schedule the Right Consultation—and Know When a Second Opinion Makes Sense
When it makes sense to stay with your current cardiologist
Stay if they:
-
Listen carefully and don’t minimize symptoms
-
Explain reasoning clearly
-
Discuss uncertainty honestly
-
Consider advanced testing when indicated
-
Partner with you instead of lecturing you
How to request more investigation (without sounding confrontational):
“Dr. ___, I appreciate the testing we’ve done. My symptoms are continuing and affecting daily life. I’d like to discuss whether additional evaluation—like cardiac MRI or other advanced testing—could clarify what’s happening. What do you recommend and why?”
When to seek a second opinion
A second opinion is normal in complex cases. Consider it when:
-
Symptoms persist, worsen, or limit daily life
-
You keep repeating the same tests with no new insight
-
Concerns are dismissed as anxiety without a thorough differential
-
The plan is “wait six months” despite ongoing episodes
-
You’re not getting a clear explanation for the mismatch between symptoms and tests
How to request it professionally:
“Dr. ___, thank you for your care. For my peace of mind and to ensure we’re not missing anything, I’d like a second opinion—especially from a specialist in cardiac imaging. Could you provide copies of my reports and records?”
A supportive clinician will respect this.
Where to look
-
Teaching hospitals / dedicated heart centers
-
Cardiologists with cardiac imaging expertise
-
Centers with strong cardiac MRI programs
-
Clinicians who routinely manage diagnostic uncertainty
Bring:
-
Symptom diary
-
Your organized medical summary
-
Full reports (not just summaries)
-
A written question list
-
A family member/friend to take notes
Step 4: Ask the Right Questions About Cardiac MRI (CMR)
Cardiac MRI isn’t “just another test.” When appropriate, it can answer questions that ECGs, standard stress tests, and echocardiograms often can’t.
The core question
“Based on my documented symptoms, the tests we’ve done, and the ongoing uncertainty—would a cardiac MRI provide information that could change how we manage my care?”
If your doctor says “not necessary”
“Can you explain what diagnoses a cardiac MRI would be most useful for in my situation—and why you feel we’ve already ruled those out?”
If your doctor says “let’s wait”
“What changes in symptoms, or what timeframe, would make cardiac MRI appropriate? What should I monitor so we don’t miss the window to act?”
If your doctor says “yes”
“What specific information are we looking for—and how would different findings change the plan?”
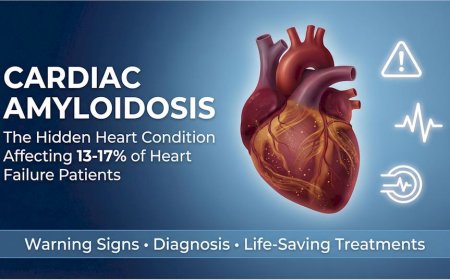
What cardiac MRI can show (in the right clinical context)
-
Tissue characterization: scarring/fibrosis with late gadolinium enhancement (LGE)
-
Inflammation: myocarditis patterns using modern mapping techniques
-
Precise structure and function: volumes, wall thickness, regional motion
-
Cardiomyopathy differentiation: ischemic vs non-ischemic patterns
-
Infiltrative processes: e.g., amyloidosis or sarcoidosis evaluation (when suspected)
-
Pericardial disease and some congenital abnormalities
It’s often considered when symptoms persist despite “normal” standard testing, when there’s concern for myocarditis/cardiomyopathy, when echo findings are borderline, or when family history raises the stakes.
Step 5: Trust Yourself—And Escalate Responsibly When Something Still Feels Wrong
The trap many patients fall into
-
Symptoms → tests → “normal” → reassurance
-
Symptoms continue → repeat basics → “still normal” → “maybe stress”
-
Symptoms worsen → still no clear answer → you start doubting yourself
Stop there.
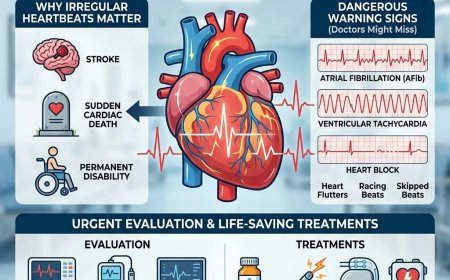
Your symptoms are clinical information. They matter—especially when they are reproducible, progressive, or function-limiting.
“Normal” tests don’t always mean “nothing is wrong”
-
An ECG is a snapshot in time.
-
A standard exercise treadmill ECG stress test has imperfect sensitivity; its ability to detect coronary disease varies by age, sex, baseline ECG, medications, and how much disease is present.
-
An echo is excellent for structure and pumping function but generally cannot characterize myocardial tissue the way MRI can.
This doesn’t mean the tests were useless. It means they are pieces of a puzzle.
Red flags that warrant prompt reassessment
Do not accept vague reassurance if:
-
Symptoms are worsening or more frequent
-
Symptoms are predictable and reproducible (e.g., exertional chest pressure that resolves with rest)
-
There is strong family history of early heart disease or sudden death
-
Multiple clinicians give contradictory explanations with no unifying plan
-
You’re told “anxiety,” but symptoms are not correlating with stress or not improving with appropriate treatment
-
Quality of life is declining because you’re avoiding activity out of fear
What “advocating” can sound like
“I understand anxiety can contribute, and I’m open to addressing that. But given my symptom pattern and how it’s affecting daily life, I’m not comfortable stopping here. I’d like a more definitive cardiac evaluation plan—either advanced imaging like cardiac MRI or referral to a cardiac imaging specialist. What are our options?”
That’s not being difficult. That’s being responsible.
Your Action Plan for This Week
Within 24 hours
-
Start the symptom diary
-
Book a follow-up appointment (or begin scheduling a second opinion)
-
Create your one-document history + medication list + family history
Within 7 days
-
Request full test reports (actual written reports, not just “normal”)
-
Continue daily documentation
-
Prepare questions for your clinician
-
Bring a support person to your visit if possible
At your consultation
-
Present your diary and organized summary
-
Ask directly whether additional evaluation (including CMR) would change management
-
Leave with a clear next-step plan: what, when, and why
The Bottom Line
Standard cardiac tests are appropriate and highly valuable for many patients. But when symptoms persist and the story doesn’t match the results, it’s reasonable to reassess, broaden the differential, and consider advanced evaluation.
You deserve:
-
To be heard
-
To have symptoms taken seriously
-
A clear plan—not vague reassurance
-
Appropriate escalation when clinically indicated
Professional Support Options
If you're experiencing possible cancer symptoms, seeking a second opinion, or unsure which tests or treatments are right for you, don't wait. Speak with a qualified oncologist today.
Connect with experienced U.S.-based cancer specialists for a comprehensive second-opinion consultation. They will carefully review your case and help determine the most appropriate next steps for your individual health needs:
👉 https://myamericandoctor.com/our-doctors/
You may also choose to enroll in our upcoming concierge medical clinic in India, Global Concierge Doctors. We offer U.S.-style primary care with 24/7 access to India-based physicians for ongoing guidance on any health concern. When required, we coordinate referrals to trusted specialists in India and the U.S. for advanced evaluation and care.
Your health decisions today shape your life tomorrow.
Medical Disclaimer
This article is provided strictly for educational, informational, and awareness purposes only. It is not intended to be, and should not be construed as, professional medical advice, diagnosis, treatment, or a substitute for consultation with qualified healthcare professionals.
No Doctor–Patient Relationship
The information presented in this article does not establish a doctor-patient relationship between the reader and the author, publisher, or any affiliated entities. No medical decisions should be made based solely on the content of this article.
Consult Qualified Medical Professionals
If you are experiencing chest pain, shortness of breath, unexplained fatigue, fainting, new palpitations, or any other concerning symptoms, seek prompt evaluation by qualified clinicians. For severe, sudden, or worsening symptoms, seek emergency care.
Individual Medical Situations Vary
Every person’s medical history, risk factors, and circumstances are unique. Diagnostic tests and treatment choices must be tailored through direct consultation with licensed healthcare professionals.
Not a Recommendation for Specific Tests or Treatments
References to cardiac MRI, ECG, stress tests, echocardiograms, or other diagnostics are informational only and do not constitute a recommendation that you should or should not undergo any specific test. Decisions must be made with your treating clinicians.
No Guarantee of Accuracy or Completeness
Medical knowledge evolves. While care has been taken to ensure accuracy, information may not reflect the most current research, guidelines, or regional practice patterns.
Third-Party Resources and Links
Any third-party services or links are provided for informational purposes only and do not constitute endorsements. The author and publisher are not responsible for the content, services, or practices of third-party entities.
Limitation of Liability
To the fullest extent permitted by law, the author, publisher, and affiliated entities disclaim liability for any outcomes arising from use of, or reliance on, information contained in this article.
Geographic and Regulatory Considerations
Regulations, standards of care, insurance coverage, and test availability vary by region and country. Information may not apply universally.
Acknowledgment
By reading and using the information in this article, you acknowledge that you have read, understood, and agreed to this disclaimer in its entirety. You further acknowledge that this article has been created with the assistance of artificial intelligence. While every effort has been made to ensure accuracy, AI-generated content may occasionally contain errors, omissions, or inaccuracies. The information presented here is intended solely for educational and informational purposes and should not be relied upon as a substitute for professional medical advice. Readers are strongly encouraged to consult qualified healthcare professionals, refer to peer-reviewed medical literature, and cross-reference information from established clinical sources before making any health-related decisions.
What's Your Reaction?
 Like
0
Like
0
 Dislike
0
Dislike
0
 Love
0
Love
0
 Funny
0
Funny
0
 Angry
0
Angry
0
 Sad
0
Sad
0
 Wow
0
Wow
0